The Prostatectomy corresponds to a minimally invasive or fully invasive procedure for the complete or partial removal of the prostate. Partial prostatectomy can be indicated as micturition disorders, whereas malignant tumors of the prostate require complete removal. In the case of complete prostatectomies, nerve injuries during the operation can cause impotence.
What is the prostatectomy?
The prostate corresponds to an accessory sex gland and is involved in sperm production. In humans, the organ lies below the urinary bladder, where it covers the beginning of the urethra down to the pelvic floor. The exocrine gland has excretory ducts into the urethra and contains up to 50 tubuloalveolar single glands.
A secretion is created in these glands, which is released into the urethra and mixes with the sperm during ejaculation. The prostate secretion has a pH value of 6.4 and thus increases the chances of survival of sperm in the acidic environment of the vagina. The prostate secretion also triggers movement on the sperm. Under certain circumstances, partial or complete removal of the prostate may be necessary. Doctors refer to such an operation as a prostatectomy or Prostate enucleation. A distinction is made between partial removal of the prostate and radical prostatectomy.
Both interventions can correspond to different surgical procedures. In addition to laperoscopic and endoscopic prostatectomies, there are, for example, robot-assisted interventions.
Function, effect & goals
The most common indication for removal of the prostate is prostate cancer. This malignant cancer of the prostate gland usually requires a radical prostatectomy. During this procedure, the prostate is completely removed. The vesicle glands (vesiculae seminalis) and the prostate capsule (capsula prostatica) are also removed in the invasive procedure.
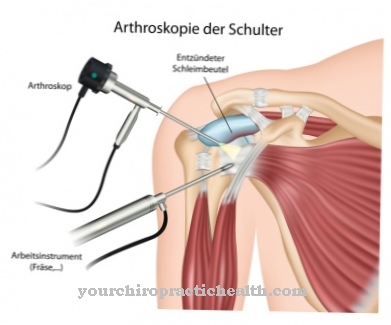
The operation can be minimally invasive and thus correspond to an endoscopy. Such an operation is known as an endoscopic extraperitoneal radical prostatectomy (EERPE). A camera in the pelvic area helps to closely monitor the surgical field during the procedure. However, the surgical procedure is almost exclusively suitable for locally limited prostate carcinomas. Laparoscopic prostatectomy is also a minimally invasive form of prostatectomy. In this procedure, access is via five trocars in the lower abdomen. The seminal vesicles and prostate are exposed during the operation with laparoscopic instruments and then removed.
Bleeding can be stopped with bipolar coagulation.A direct suture of the anastomosis between the urethra and the bladder stocking is common. If necessary, the iliac lymph node packages are also removed. Depending on the indication in the individual case, the treating surgeon performs the operation transperitoneally or extraperitoneally without manipulating the peritoneum. In addition to partially invasive access procedures, there are also open access routes for prostatectomy. One such procedure is retropubic radical prostatectomy (RRP), in which the patient lies on their back with their legs apart. The surgeon removes the prostate through a median incision between the navel and symphysis.
He then freely prepares the prostate and supplies the vascular plexus with puncture sutures. The retropubic approach leaves the organ capsule untouched and is usually used to remove large adenomas. The simultaneous removal of the seminal vesicles and lymph nodes is also conceivable with this open procedure. This type of prostatectomy is the most frequently used worldwide. Radical perineal prostatectomy (RPP) is also an open variant of prostatectomy. The surgeon looks for the prostate through an incision between the anus and scrotum and prepares the gland with metal retractors inserted urethrally. Very enlarged prostates cannot be operated on with this procedure.
Partial removals of the prostate are mostly used for benign tumor diseases of the gland, if these are accompanied by problems with urination. One example of a partial removal procedure is transurethral prostate resection (TURP), which involves inserting a surgical instrument through the urethra. The surgeon removes certain parts of the gland from the transitional zone of the prostate with a loop-shaped electrode including HF alternating current. The prostate capsule is retained. Related procedures are transurethral microwave thermotherapy and photoselective vaporization of the prostate (PVP).
You can find your medication here
➔ Medicines for bladder and urinary tract healthRisks, side effects & dangers
The risks and side effects of prostatectomy depend on the procedure chosen. Radical prostatectomies are relatively difficult operations because of the anatomical conditions, regardless of how they are performed. The prostate is difficult to access in the pelvis. Branches of the cavernous nerve are only millimeters away.
The nerve bundles carry nerve fibers for erection. If these fibers are accidentally cut or severely stretched, there is a loss of erectile function. A previously common side effect of radical prostatectomies was urinary incontinence, which has now fallen far behind impotence. In addition, the penis can shorten during the operations, as the urethra is connected at the severed ends after the excision of individual parts. The penis is pulled a little way into the body to compensate for the urethral losses. The foreskin usually retains its conventional shape and is often too long after the operation, which can promote chronic inflammation of the glans.
Another common side effect of radical retropubic prostatectomy is the inguinal hernia, which requires repeated surgery. In addition to these side effects and risks, there are general anesthetic and surgical risks. In addition to infections, these include bleeding and bruising. Post-procedure pain is also common. For people with cardiovascular diseases, open procedures with general anesthesia are a heavy burden on the system, which in extreme cases can lead to cardiovascular arrest. Allergic reactions to the anesthetic are also among the general surgical risks. The same applies to wound healing disorders or headaches in response to the anesthetic.











.jpg)



.jpg)










.jpg)
