The Pudendal neuralgia is a rare disease that causes severe pain in the genital area and perineal region, sometimes shooting in a flash. The disease is preceded by mechanical or inflammatory damage to the pudendal nerve. The aim of therapy is to regenerate the nerve in order to alleviate the symptoms.
What is pudendal neuralgia?

© pixdesign123 - stock.adobe.com
The designation Pudendal neuralgia is formed from the stems pudendus and neuralgia. Neuralgia is the term used to refer to nerve pain that shoots in like a attack, pudendus refers to the pudendal nerve.
This originates in the lower spinal cord. It has three branches that innervate the anus, the external anal sphincter, the perineum, the muscles of the penis roots, the urethral muscle, the glans penis and the labia with clitoris. The pudendal nerve is also responsible for controlling the pelvic floor muscle.
Patients describe the pain that can extend into the abdomen or the soles of the feet as pinprick, stabbing, pulling or burning. The skin in these regions is very sensitive to pain and extremely sensitive. The pudendal neuralgia is to be differentiated from the pudendal neuropathy, in which permanent symptoms occur.
causes
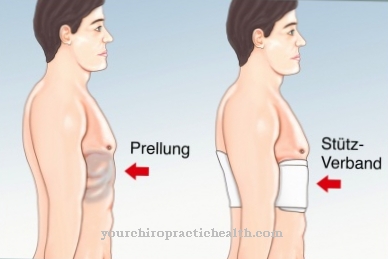
The most common cause of Pudendal neuralgia is the mechanical damage and thus narrowing of the pudendal nerve. The causes are lengthy operations in the lower pelvis, long pressure on the nerve, as can occur when cycling, and injuries. In some patients, a narrowing of the connective tissue canal on the spine was demonstrated.
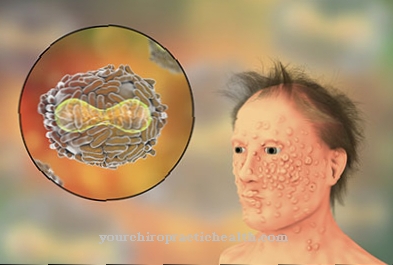
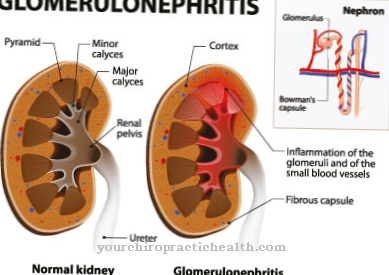
More rarely, pudendal neuralgia is caused by inflammation of the nerve. These arise from herpes zoster viruses, tumors in the pelvic region or from diabetic nerve diseases. Diabetic polyneuropathy is the most common cause of inflammation and the result of poorly controlled diabetes mellitus or damage to the small blood vessels. Diabetics therefore represent a special risk group for neuralgia.
Symptoms, ailments & signs
Typical of pudendal neuralgia are violent pain in the genital area that occurs suddenly and is described by those affected as stabbing, burning or pressing. In women, they usually extend from the external vagina to the anus; Men feel the pain mainly in the perineal area, the penis can also be affected.
The symptoms usually occur on one side, but can change sides - only occasionally do the pain symptoms occur on both sides at the same time. The pain, which is perceived as very excruciating, is sometimes associated with sensory disturbances or muscle paralysis, which can have a massive impact on bowel movements and urination. In severe cases, pudendal neuralgia can cause urinary and fecal incontinence.
The pain often occurs during sexual intercourse and lasts for a while afterwards, and erectile dysfunction occasionally occurs in men. As a rule, the discomfort worsens when sitting, which is often only possible with the help of a seat ring.
Sports activities as well as long standing lead to a worsening of the pain symptoms, while sitting on the toilet leads to a relief for the patient. The symptoms also subside when lying down, and undisturbed sleep is generally possible. The disease often takes a chronic course, as the pudendal neuralgia hardly responds to the usual painkillers.
Diagnosis & course
When diagnosing the Pudendal neuralgia the doctor must first rule out other conditions that could cause pain in the affected area. This includes in particular skin inflammation. Diabetes mellitus must also be ruled out on the basis of a blood test.
A tumor is examined using imaging techniques. The question of the psychological causes of pain in the genital area is also standard. If these factors could be excluded, further diagnostics will be carried out by a neurologist. Based on the anamnesis and clinical examination, the doctor usually receives sufficient clues for diagnosis, which he can support using technical examination methods.
However, measuring the nerve conduction velocity of the pudendal nerve or measuring the electrical activity in the external anal sphincter are rarely effective.
Another diagnostic method is the injection of a local anesthetic into the nerve canal during a computed tomography scan. If the pain then clearly subsides, pudendal neuralgia must be diagnosed.
Complications
Because of the pudendal neuralgia, those affected usually experience very severe pain. These pains occur mainly in the intestines or genitals and are very uncomfortable for most of those affected. If this pain persists over a longer period of time, it can lead to psychological complaints or even depression.
Most patients often appear irritated or slightly aggressive. Sometimes the pain expresses itself as burning or stabbing. In some cases, this can lead to restricted mobility and inflammation of the skin. Certain activities in everyday life are no longer possible for the patient without further ado or are always associated with severe pain.
If treatment is not available, the nerve can be irreversibly damaged by the pudendal neuralgia. Treatment of pudendal neuralgia is carried out with the help of drugs. There are no complications. However, regeneration of the nerve is also necessary so that the pain does not recur. Pudendal neuralgia does not usually reduce the patient's life expectancy.
When should you go to the doctor?
Pudendal neuralgia should always be evaluated and treated by a doctor. In most cases there is no self-healing and pudendal neuralgia cannot be treated by self-help measures. Medical treatment is therefore essential. A doctor should be consulted if the person concerned suffers from lightning-like and very strong, stabbing pain. This pain can occur in different situations and also in different parts of the body. However, this pain mostly occurs in the bowel and upper abdomen area. Pudendal neuralgia can also lead to urination problems, and patients often show paralysis of the muscles or even erectile dysfunction. A doctor must also be consulted with these complaints.
The initial diagnosis of pudendal neuralgia can be made by a general practitioner or by a urologist. However, further treatment is carried out by a specialist doctor.
Treatment & Therapy
The injection of local anesthetics is not only used for diagnosis, it is also the most important therapy for Pudendal neuralgia. Since the effect usually wears off after a few weeks, continuous supply using a catheter can also be provided. In some cases, cortisone is given instead of local anesthetics.
Most doctors initially prefer drug therapy to this method, as the active ingredient is taken regularly. The drugs used are tricyclic antidepressants, which have been successful in treating nerve pain even in low doses, and anti-epileptic drugs.
Some neurologists are of the opinion that only a combination of the two drugs promises long-term therapeutic success. The transcutaneous electrical neurostimulation (TENS) in the genital area, which the patient regularly performs at home, also promises good prospects for healing.
Treating the underlying disease is also important, but not the only measure in advanced disease. The last option after failure of all drug and non-drug conventional medical therapies is surgery. In so-called neurolysis, an attempt is made to expose the nerve in its canal and thus free it from mechanical pressure.
In addition to conventional medicine, those affected can also find help in traditional Chinese medicine with relaxation exercises and acupuncture.
You can find your medication here
➔ Medicines for painprevention
Due to the wide range of causes, it is not possible to make predictions about the course of the disease, and preventive measures can be named. Timely, also psychological, care is important in order to counteract chronicity. A healthy lifestyle with sufficient exercise also seems helpful.
Pudendal neuralgia has different causes. The acute treatment must relieve pain, but also relate to the underlying disease. Therefore, aftercare for pudendal neuralgia is very individual. Often, repeated pudendal blockade helps relieve the pain. The long-term success of the treatment must be secured and checked during aftercare.
If the illness is long-term, therapy with stronger pain relievers may be necessary. Follow-up care then primarily concerns a good setting of the medication in order to maintain freedom from pain, as well as the observation of side effects of these medications. The pain relievers often have to be taken over a long period of time and the dose must be individually adjusted to the patient under certain circumstances.
Long-term and supportive, after the acute treatment of pudendal neuralgia, consideration can be given to using accompanying measures that can help alleviate the symptoms. Above all, the psychological accompaniment of pain therapy by learning and applying relaxation methods should be mentioned here. Further supportive therapy measures such as TENS, acupuncture and homeopathic remedies should be considered by a qualified doctor and presented to the patient.
You can do that yourself
The treatment of pudendal neuralgia can be supported by the sufferer through dietary measures and a general change in lifestyle. Which steps make sense in detail depends primarily on the causal disease and the advice of the doctor. If the symptoms are caused by diabetes mellitus, the doctor will recommend an appropriate insulin medication, which can be supported by a change in diet. If the cause is a tumor in the pelvis, it must first be removed. After the surgical removal of the tumor, bed rest is initially applied.
The sick person should also visit the doctor regularly so that any recurrences or other complications can be identified quickly. In addition to paracetamol and the like, natural pain relievers such as St. John's wort or aloe vera also help with acute pain attacks. In addition, anticonvulsants should be taken, such as sage and various herbal teas.
Various relaxation methods are also available. This includes measures such as yoga and physiotherapy, but also osteopathy, homeopathy and acupuncture. Pudendal neuralgia can be treated well using these measures. In individual cases, such as severe pain or side effects that make physical activity impossible, home remedies should be avoided. The patient must then strictly adhere to the medical guidelines and, if necessary, be treated in a hospital.

.jpg)