Of the Edge current Of the blood, the bloodstream is in close proximity to the walls of the vessels. In the smaller vessels in particular, there is a plasmatic marginal current without leukocytes and erythrocytes, which has a significantly lower flow rate than the central bloodstream. The marginal current changes with inflammatory reactions.
What is the edge current?
.jpg)
Medicine understands the marginal flow of blood to be a phenomenon within the Fåhraeus-Lindqvist effect. This effect is a foundation of blood flow which relies on the fluidity of the red blood cells and affects the viscosity of the blood. Because of the Fåhraeus-Lindqvist effect, the viscosity in the vessels of the periphery is significantly lower in vessels with a small lumen than in vessels with a higher lumen.
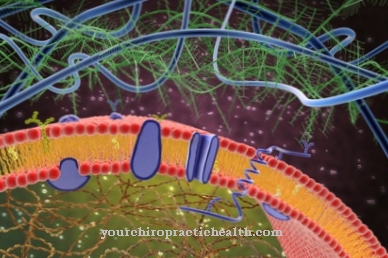
In the vicinity of the vessel walls, shear forces act on the red blood cells. The resulting shear forces displace the erythrocytes and cause the red blood cells to migrate axially, which creates an axial current. Simultaneously with the axial migration of the red blood cells, cell-poor marginal currents develop near the vessel walls. The marginal currents from plasma wash around the cells and act as a kind of sliding layer for the blood cells in the Fåhraeus-Lindquist effect.
In larger vessels, the plasmatic marginal current can be neglected, as it only takes up a small proportion of the vessel cross-section. Only in pre- and post-capillary vessels with a small cross-section does it make up a significant part.
Function & task
The marginal flow of blood can be observed in all vessels, as shear forces are effective in the areas near the vessel walls. However, from a medical point of view, the marginal current in vessels with a larger lumen is not as relevant as in vessels with a smaller cross-section. In small cross-sections, the shear forces acting on the walls cause the individual components of the blood to redistribute. In this context, the blood is to be regarded as a suspension, the largest particles of which migrate into the faster flowing axial flow due to the shear forces.
The leukocytes are the largest part of the blood. After migration, you are in the immediate center of the axial flow. The erythrocytes move somewhat more peripherally. The platelets move even further in the periphery. In vessels with a small diameter, with normal blood flow, a marginal flow of pure plasma is created that hardly contains any blood cells.
The blood flow is determined by the laws of hemodynamics. These include Darcy's law and the Hagen-Poiseuille law. For this reason, the flow behavior of blood depends primarily on blood pressure, vascular resistance and blood viscosity.
Blood is an inhomogeneous suspension of blood plasma and blood cells. The blood viscosity does not follow a constancy, but depends on the flow velocity and increases with slow blood flow. Especially the erythrocytes of the blood tend to aggregate at low shear rates. As soon as the blood reaches a faster flow rate, the aggregates break open. This creates a non-proportional, erratic flow behavior that turns the blood into a non-Newtonian fluid.
This relationship is only relevant in the smaller vessels. In larger vessels, the blood behaves more or less like Newtonian fluid. The speed of the peripheral flow of blood always lags behind the central flow. Occasionally, blood is also referred to as double-flow behavior, which is composed of the edge flow close to the wall and the central flow. The composition of the peripheral flow and central blood flow differs depending on the vessel diameter. Basically, platelets tend to move in the marginal flow, whereas leukocytes tend to move in the central flow.
Illnesses & ailments
Under pathological conditions, however, it can happen that leukocytes preferentially move in the marginal stream of the blood. This phenomenon makes up the so-called sludge phenomenon, for example. In the sludge phenomenon, the erythrocytes of the blood accumulate in the context of microcirculation disorders. One consequence of this erythrocyte aggregation is a slower flow rate and a subsequent reduced oxygen supply to affected tissues. Any type of restricted blood flow within the smallest blood vessels is considered a microcirculatory disorder.
Microcirculation disorders affect the supply of nutrients to the tissues in addition to oxygen. The disturbances are caused by restricted blood flow or a disturbed exchange of substances within the blood vessels with a diameter of less than 100 µm. In addition to the rheological properties of blood, microcirculation is primarily dependent on blood pressure and ultimately the diameter of the blood vessels. However, these factors are prone to failure. If there is insufficient drainage in the venous system, the blood backs up in the capillary bed and the blood flow is disturbed. In this way, microcirculation disorders arise with an unusual flow distribution of the blood cells.
Diseases or pathological phenomena with symptomatic microcirculation disorders can, for example, be acute inflammatory reactions. In addition, the circulatory disorders occur in the context of PAOD (peripheral arterial occlusive disease), CHD (coronary heart disease) and the tropical ulcer with insufficiency of the veins.
The same goes for gangrene. If there are many leukocytes in the marginal stream of the blood and the blood flow velocity has decreased, the leukocytes from the marginal stream adhere to the vessel walls. However, this adhesion is reversible. As soon as the flow rate increases again, the leukocytes are detached from the walls of the vessels and carried on.
A changed marginal flow of the blood can also be the result of arteriosclerotic changes within the blood vessels. In arteriosclerosis, the vessels calcify. Various components are deposited on the vessel walls and thus increasingly narrow the lumen of the affected veins.




.jpg)





















