A Rectal prolapse or. Rectal prolapse occurs when part of the colon from the lowest section (rectum) slips out of the muscular opening at the end of the digestive tract (anus). Surgery is usually needed to treat rectal prolapse.
What is rectal prolapse?
.jpg)
© nmfotograf - stock.adobe.com
A Rectal prolapse is a rare disease and mainly affects the elderly. The disease is rather rare in children; affected children are usually younger than 3 years. Men are much less likely to develop rectal prolapse than women (80-90% probability).
The disease affects the rectum, i.e. the last 12-15 inches of the colon just above the anal canal. Usually the rectum is securely attached to the pelvis with ligaments and muscles. Various factors, such as age, long-term constipation, or stress during childbirth, can weaken it. This causes the rectum to prolapse, i. falls out of its natural body opening (rectal prolapse).
A rectal prolapse must be distinguished from a rectocele, which is a bulging of the rectum into the vaginal walls. Another form of rectal prolapse is called intussusception. One section of the intestine turns inside another, which can lead to an intestinal obstruction.
causes
A Rectal prolapse is caused by a weakening of the muscles that hold the rectum in place. Most people with rectal prolapse also have weak anal sphincters.
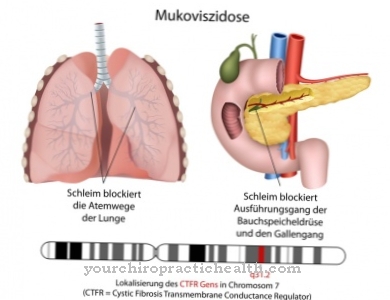
The exact cause of this weakening is unknown, but risk factors for rectal prolapse are usually advanced age, prolonged constipation or persistent diarrhea, straining during bowel movements, pregnancy, and stress during childbirth. Rectal prolapse can also be caused by previous operations, cystic fibrosis or chronic diseases.
These include lung diseases, whooping cough, multiple sclerosis and long-term hemorrhoidal diseases. Children who have had rectal prolapse should also be evaluated for cystic fibrosis, as this can be a symptom of the disease.
Symptoms, ailments & signs
Rectal prolapse manifests itself through several symptoms, whereby a slight and incomplete prolapse can easily be mistaken for hemorrhoidal disease. The main symptom of a rectal prolapse is the rectum that has come out and turned outwards. A distinction is made between a rectum that has just stepped outwards and the presence of intussusception. The latter means an invagination in itself, whereby an invagination of the intestine in itself can also lead to a prolapse.
Since the mucous membranes of the intestine get to the outside, those affected feel a permanent feeling of moisture. Sometimes bleeding occurs because the leaked rectum is injured by clothing or manual manipulation. A foreign body sensation on the anus is often described by those affected. Itching often occurs, which can sometimes be explained by inflammation.
A rectal prolapse almost always leads to symptoms of incontinence. This can lead to the uncontrolled discharge of feces or mucus. The more severe the incident, the more pronounced the incontinence. Complete rectal prolapse almost always means faecal incontinence. An only partially existing prolapse, however, does not necessarily mean fecal incontinence, but does lead to the loss of mucus. A rectal prolapse can also be clearly identified optically.
Diagnosis & course
In the early stages of one Rectal prolapse the rectum slowly loosens, but remains in the body. This stage of rectal prolapse, when the connective tissue of the rectal lining becomes loose and protrudes from the anus, is known as mucosal prolapse.
The further the rectum prolapses, the harder a part of the rectum presses on the anus and weakens it. This stage is called complete rectal prolapse and is the most common diagnostic stage of the disease. Symptoms of rectal prolapse are similar to those of hemorrhoids, ranging from painful bowel movements, mucus, or blood from the protruding tissues, to fecal incontinence or loss of urgency.
To diagnose an earlier stage when the rectum has not yet protruded from the anus, doctors may give a phosphate enema to differentiate rectal prolapse from protruding hemorrhoids. Using a dynamic MRI, the entire pelvis including the pelvic floor muscles and pelvic organs can be scanned during bowel movements.
Complications
A prolapse of the rectum or rectal prolapse almost always requires surgical treatment to avoid complications. Operations are usually not necessary in children. Most of the time, however, older people suffer from rectal prolapse. Due to the progressively increasing weakness of the connective tissue, self-healing no longer takes place here.
If the rectal prolapse occurs in children, there is usually another serious illness behind it, which also promotes the development of complications. Affected children should be examined for cystic fibrosis, among other things. In the much more common cases of rectal prolapse in older people, complications will always develop over time if the condition is left untreated.
However, life-threatening complications are the exception. Clamping of the rectum usually does not occur because the bowel can be pushed back again and again. However, this can happen in exceptional cases. This is then a life-threatening emergency that requires immediate surgical intervention in order to avoid the death of the corresponding section of the rectum.
In the other cases, there is no emergency, but a surgical procedure is still necessary, because an untreated rectal prolapse leads in the long term to increasing pain during bowel movements and blood and mucus on the stool, as well as fecal incontinence. The later the treatment, the more serious the associated complications. Ulcers can also develop in the rectum area.
When should you go to the doctor?
A skilled doctor can spot a rectal prolapse at a glance. Rectal prolapse, also known as extended anal prolapse, is often found in older women. It is imperative to see a doctor, as parts of the intestine have leaked through the anal opening.
The preliminary stages of this phenomenon were mostly ignored and triggered by pressing too hard on the toilet. They may not be noticed because often only a few wrinkles of the rectum are protruding. Therefore, a visit to the doctor is often omitted if there are minor symptoms. However, the rectal prolapse cannot go unnoticed as an advanced anal prolapse.
Rectal prolapse can occur from heavy lifting or a coughing fit. If left untreated, the rectal prolapse remains permanent. He needs surgical treatment. In the case of a prolapsed rectum, larger parts of the rectum and rectum have already leaked out through a weak pelvic floor or as a result of an illness. The result is that the stool can no longer be held in the bowel. Intestinal incontinence occurs.
Before a rectal prolapse occurs, a doctor should be considered. Treatment options are greater the earlier treatment is started.If you keep getting the feeling that something has happened in the anus after a bowel movement, your visit to the doctor should no longer be postponed. For prophylaxis, women over 40 should start with pelvic floor exercises.
Treatment & Therapy
Almost all cases one Rectal prolapse need medical care. Occasionally, successful treatment of the underlying cause of rectal prolapse solves the problem; in most cases, rectal prolapse will get worse without surgery.
In infants and young children, reducing or thinning bowel movements under the guidance of a doctor can help. Medical treatment begins to temporarily relieve symptoms of rectal prolapse or to prepare the person for surgery. Fillers (bran, psyllium, methylcellulose or psyllium), stool softeners or enemas are used for this.
The goal of all surgical techniques for correcting rectal prolapse is to reattach the rectum to the inner pelvis. This procedure under general anesthesia is carried out through the abdominal wall in healthy and younger patients and through the perineum in older people or in poor health, which generally requires a hospital stay of three to seven days.
prevention
A high-fiber diet and an adequate supply of fluids every day can increase the risk of developing constipation and thus a risk factor for one Rectal prolapse to reduce. Biofeedback therapies train the pelvic floor muscles and strengthen the sphincter. People with persistent diarrhea, constipation, or hemorrhoids should treat them in good time to reduce the risk of rectal prolapse.
Aftercare
Rectal prolapse requires consistent follow-up care, regardless of whether it has been treated conservatively or surgically. In essence, it is important to prevent the condition from recurring or worsening. For this purpose, the gastroenterologist and proctologist, but also the family doctor, are the specialist contacts. There are also self-help groups for people with proctological diseases who can offer empathetic exchange of experiences and helpful tips.
In the follow-up of rectal prolapse or rectal prolapse, stool regulation is particularly important. Pressure during bowel movements must be avoided in any case. A (not too) soft and voluminous chair is ideally suited to avoid pressing. Fruits and vegetables are suitable here, especially fiber in the diet.
It is essential to ensure that there is a sufficient drinking menu (usually around 1.5 to 2 liters of water or herbal tea). If this diet is not sufficient to regulate the stool, natural helpers can be used with psyllium husks. It is better to avoid constipating foods such as chocolate or eggs for a while.
Movement is also important for stool regulation. Light endurance sports and walking are recommended in this context. Exercise and yoga can also activate bowel movements. Long periods of sitting on the toilet should be avoided, as should too active pressing.
You can do that yourself
Rectal prolapse or rectal prolapse is a disease, the diagnosis and treatment of which belongs in professional hands. Nevertheless, self-help by patients in everyday life is possible and also desirable. The active cooperation of the patient can prevent the rectal prolapse and support both therapy and aftercare in a targeted manner.
In many cases, rectal prolapse is caused by strong pressure during bowel movements and a weakness of the connective tissue in the area of the pelvic floor. This is where self-help can begin in a targeted manner. It is essential to avoid constipation, so that stool regulation plays an important role in the patient's everyday life. This is achieved through a high-fiber diet combined with a sufficient amount of water. As far as possible, constipating food should be deleted from the nutrition plan. A lot of exercise is also important, as physical activity stimulates the intestinal activity of those affected and can thus have a positive effect on rectal prolapse. Massages of the abdominal area and warm baths for constipation are also recommended, as are flea seed preparations.
The pelvic floor can be well trained with suitable exercises. The exercises are taught by the physiotherapist or the treating doctor and can be performed daily at home. Regular check-up visits to the doctor are also important if a rectal prolapse has been diagnosed and treated. Shame is a major obstacle to discovering an incident (including a relapse) as soon as possible and treating it promptly and effectively.





















.jpg)


