At a respiratory failure there is a reduced ventilation of the alveoli due to a disturbance of the external breathing. Those affected suffer from shortness of breath, coughing and poor performance.
What is respiratory failure?

© Morphart - stock.adobe.com
The respiratory failure is also known as Respiratory failure designated. The gas exchange in the lungs is disturbed. This leads to abnormally changed blood gas values. A distinction can be made between acute and chronic insufficiency. The symptoms of acute insufficiency are similar to those of chronic insufficiency. However, they set in much more suddenly and are therefore often associated with a severe panic reaction.
In addition, the insufficiencies can be divided into partial and global insufficiencies according to their extent. Respiratory insufficiencies are not diseases in their own right, but rather a complex of symptoms that are caused by various other diseases. The insufficiency is therefore always treated by treating the underlying disease. However, oxygen administration can improve symptoms.
causes
The causes of respiratory failure are obstructive and restrictive ventilation disorders of the lungs. In the case of restrictive ventilation disorders, the lungs are no longer sufficiently expandable; this can also apply to the chest. This leads to a decreased lung volume. In particular, the vital capacity, the functional residual capacity and the residual volume are limited. Restrictive ventilation disorders can occur if the chest is deformed.
The most common causes of such a chest deformation are trauma or scoliosis. Reduced ventilation of the alveoli in the case of pneumonia can also lead to a restrictive ventilation disorder. Adhesions in the chest (e.g. pleural rinds), pulmonary edema or neuromuscular diseases can also reduce the elasticity of the lungs and chest.
When there is an obstructive ventilation disorder, the flow resistance in the airways is increased. This increases airway resistance, functional residual capacity and residual volume. The alveoli are not evenly ventilated, so that the lungs over-inflate in the long term. In addition, the entire lung and bronchial system is mechanically damaged.
In the long run, this reduces the vital capacity of the lungs. An obstructive ventilation disorder is associated with bronchial asthma, cystic fibrosis, emphysema or chronic obstructive pulmonary disease (COPD). Acute respiratory failure is usually caused by pneumonia, aspiration of water or foreign bodies, or injuries to the lungs and chest.
A disruption of the respiratory center in the brain can also lead to acute respiratory failure. Chronic respiratory failure is more likely to be caused by chronic lung disease or cancer. Even after the surgical removal of a lung (pneumectomy) or a lobe of the lung (lobectomy), respiratory insufficiency can develop.
Symptoms, ailments & signs
In partial insufficiency, the partial pressure of oxygen in the arterial blood system drops. The carbon dioxide partial pressure can, however, still be compensated, so that only hypoxemia but not hypercapnia occurs. In global respiratory failure, hypoxemia is also accompanied by hypercapnia. This means that the oxygen content in the blood is reduced, but the carbon dioxide partial pressure is increased.
In acute respiratory failure, symptoms appear suddenly. Those affected suffer from attack-like shortness of breath with a feeling of suffocation. The acute asthma attack with coughing and difficult exhalation is also a temporary respiratory failure. If the respiratory center is damaged, however, there is no shortage of breath. Instead, the affected people become unconscious immediately and die quite quickly without treatment.
Chronic respiratory failure is far more common than the acute form. Here, too, there is shortness of breath and coughing. Due to the chronic lack of oxygen, the patients are no longer as productive. A blue discoloration of the skin (cyanosis) may be observed. Symptoms such as drumstick fingers or watch glass nails can occur with longer courses.
Diagnosis & course of disease
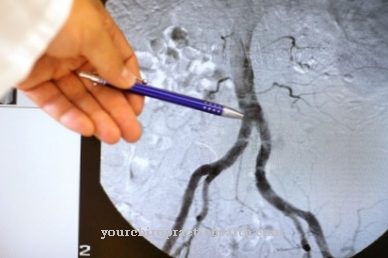
At the beginning of the diagnosis, patients are thoroughly examined. Auscultation and percussion of the lungs take place. Attenuated breathing noises, background noises or rattling noises may be heard here. Air-filled or dead breathing spaces can be discovered during percussion.
Imaging methods such as chest x-ray or computed tomography provide further clarity. Magnetic resonance imaging or pulmonary scintigraphy can also be performed. With the help of an endoscope, the bronchi (bronchoscopy) and the mediastinal space (mediastinoscopy) can be visualized.
The lung function diagnostic procedures can be used to determine the performance of the lungs. Important methods of lung function diagnostics are spirometry and body plethysmography. In the laboratory, partial insufficiency shows an oxygen partial pressure below 75 mmHg in the blood gas analysis. In global insufficiency, the carbon dioxide partial pressure is also above 45 mmHg. The blood gas analysis is carried out from the capillary blood after it has been removed from the earlobe.
Complications
Respiratory failure is a serious complication of lung or heart disease. It leads to an insufficient supply of oxygen to the body and especially the brain. As a result, serious and often life-threatening complications occur. The severe shortness of breath can lead to impaired consciousness and even coma. Initially, the disturbances of consciousness become noticeable in states of confusion.
It can also lead to a sharp drop in blood pressure. The heart rate is often very low. A coarse tremor of the hands (flapping tremor) is also often observed. These complications can only be prevented by artificial respiration. Chronic respiratory failure is incurable because it is based on incurable lung diseases such as emphysema, COPD or pulmonary fibrosis.
In the chronic form of the disease, long-term therapy with oxygen ventilation must therefore be carried out. Otherwise, there will be permanent impairment of brain and heart function, which can lead to long-term damage or even death. The course of acute respiratory failure can be moderate, but also very severe, depending on the cause.
Possible causes for severe acute forms include sepsis, severe heart disease, pneumonia or acute pancreatitis. Mechanical ventilation is required here to prevent severe impairment of consciousness, including coma, cardiac arrhythmias and sudden cardiac death. Otherwise, the underlying diseases play a major role in the prognosis.
When should you go to the doctor?
As a rule, this disease should always be treated by a doctor. In the worst case, the affected person can die if the disease is not treated in time. The earlier it is recognized, the greater the likelihood of a complete cure. A doctor should then cut open if the person has severe breathing difficulties. A cough develops, and the patients also appear very tired. The air you breathe can also taste like carbon.
The affected person can also completely lose consciousness due to the symptoms. If the skin turns blue or the affected person passes out, an emergency doctor should be called immediately or the hospital should be visited. First aid should be provided until the emergency doctor arrives. The disease is usually treated by an internist. Complete healing cannot be guaranteed.
Therapy & Treatment
Respiratory insufficiency can only be treated by treating the underlying disease. Oxygen may be given to make breathing easier for the affected patient. The patients may need permanent artificial ventilation.
prevention
Not all lung diseases that can cause respiratory failure can be prevented. However, there are preventable factors that can contribute to the development of lung disease.Avoiding these harmful factors can protect against pulmonary disease. The main risk factor for lung disease is smoking.
There are more than 90 harmful substances in cigarette smoke. These not only weaken the immune system, they also reduce the ability of the lung tissue to clean itself. Another risk factor for lung diseases is indoor radon. Radon is a radioactive noble gas that occurs naturally in the ground and in rocks.
Radon can penetrate living spaces through leaks in the floor area of the house. Badly insulated old buildings and houses without a base plate are particularly at risk. If the radon levels in the house are elevated, the insulation should be replaced.
Aftercare
After successful treatment of respiratory failure, it is of fundamental importance to continue treatment in order to prevent the disease from breaking out again. Breathing aids that ensure oxygen uptake and supply should therefore continue to be used even when symptoms decrease. However, the supply of oxygen should always be adapted to the oxygen content in the blood. For this purpose, it must be measured regularly by the doctor.
If another illness was the cause of respiratory failure, it must be treated further after the respiratory failure has subsided. Depending on the underlying disease, it may be necessary to take certain medications for life. Follow-up treatment should be specifically tailored to the underlying disease and discussed with the doctor.
If a lung tumor was the cause of the respiratory failure, regular lung function tests by the responsible specialist and controls of the oxygen levels in the blood are necessary even after its treatment. In addition, the development of respiratory failure should be a warning signal, especially for smokers.
For follow-up treatment it is absolutely necessary to refrain from smoking under all circumstances, as this has a lasting negative effect on lung function and oxygen uptake in the blood, but also on blood circulation. In addition, exercise and exercise can improve lung function and blood circulation and are highly recommended for follow-up treatment, as well as weight loss in overweight patients.
You can do that yourself
Regardless of the cause of the respiratory failure, patients should strictly follow the doctor's recommendations. This means that the medication is taken according to plan. If the breathing problem worsens, the next doctor's appointment is due. With a flu vaccination, those affected can protect themselves from additional complaints.
It also makes sense to take certain safety precautions for everyday situations in the car and when traveling. This prevents panic attacks even on longer journeys. Smokers who suffer from respiratory failure should definitely quit, as nicotine makes the symptoms worse. If headaches constantly occur due to shortness of breath or the ability to concentrate decreases, it makes sense to assess your own symptoms correctly and to clarify them at the next doctor's appointment. Often the respiratory failure is related to another illness. That is why it can only be successfully treated together with the cause.
Correct intake of the prescribed medication will reduce the symptoms. In the event of an acute attack, gentle breathing exercise may help combat the panic that is rising. If this does not work, artificial ventilation must be given as quickly as possible. Transportable liquid oxygen systems are available for long-term, chronic breathing difficulties, which patients should always have with them.



.jpg)


















.jpg)


