The medical professionals understand the term Retinitis inflammation of the retina of the eye. Triggered by various factors, it can lead to complete loss of vision in the further course.
What is retinitis?
At a Retinitis it is an inflammation of the retina, which is often triggered by infections. The course of the disease can be characterized by harmless symptoms, but it can also lead to complete blindness.
causes
Retinitis, in most cases, is caused by inflammation spreading to the retina. The damaged retina increasingly degenerates as the fine tissue gradually recedes. Often this inflammation is triggered by an infection.
A herpes simplex virus can be detected in the secretion of the tear fluid. It can manifest itself in the retina and trigger local inflammation, which quickly leads to blindness. Herpes simplex retinitis is often seen following HSV illness, but can occur months or years later.
Lyme disease caused by the bite of a tick is also suspected. The causes for the development are manifold. Genetic factors or massive mechanical influences also play a role
Symptoms, ailments & signs

© Artemida-psy - stock.adobe.com
The body reacts to inflammation with certain stimuli. It recognizes the harmful foreign substances and shows symptoms of inflammation such as tissue swelling, reddening or heat development up to fever. Numerous defense processes interlock. The swelling of the tissue is caused by an increased fluid content that is supposed to flush harmful pathogens out of the body.
In retinitis, for example, the reddening of the retina leads to increased blood flow and, at the same time, better supply of the tissue. The generation of heat in inflammation is an enormous effort for the organism, whereby various metabolic processes can also damage the tissue. Normally, the body repairs these after the acute phase.
If the repair of retinitis is successful, the inflammation will subside without impairment. The retina can recover and the affected eye is fully operational again. However, if the process does not react normally, permanent damage can be expected.
Diagnosis & course of disease
As soon as a suspected diagnosis has been made, the exact course of the disease in retinitis is often unclear. To do this, the respective trigger of the disease must first be determined. Furthermore, retinitis is divided into subgroups with different specifications or classifications.
There is central retinitis, which mainly affects the middle retinal area. Thus, not the entire surface of the eye is affected, but only the center of the retina. This area contains a large number of photoreceptor cells that are responsible for focusing the optical image.
A severe course of the disease of central retinitis is therefore usually associated with permanent damage and loss of vision for the middle field of vision of the affected eye. Retinitis with bleeding is known as hemorrhagic retinitis. Sepsis (blood poisoning) can lead to septic retinitis. develop and syphilitic retinitis is the result of syphilis.
Inflammation of the choroid (chlorioretinitis) is often seen in connection with exudative retinitis. Typical symptoms are pronounced water retention in the tissue (edema), and occasional bleeding. Subsequent retinal detachments show up, which immediately lead to failure symptoms in the central area of the retina.
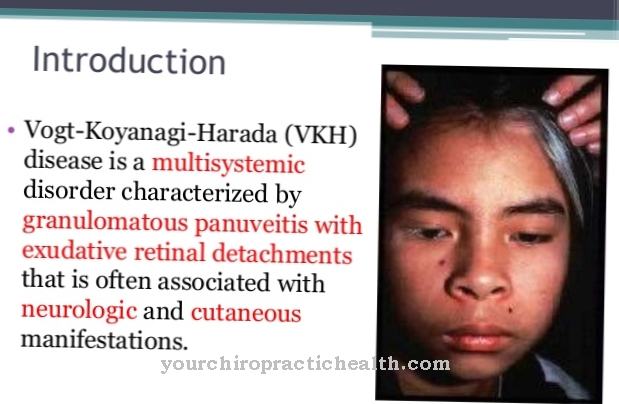
Retinitis can also trigger Harada syndrome. There is also meningoencephalitis (inflammation of the meninges and the brain). The symptoms manifest themselves in the typical imbalance, hearing problems, pigment loss and hair loss. Almost every tenth person affected does not survive the constellation of retinitis and meningoencephalitis.
Numerous examination methods are available for the determination of retinitis with its multiple manifestations. First and foremost, the eye is examined using a slit lamp for the front, middle and back of the eye. To show the background of the eye, the reflection is carried out with the help of an ophthalmoscope. The spectrum of diagnostic procedures ranges from measuring intraocular pressure and corneal topography to determining the resolution of the eye retina using a retinometer.
Complications
Retinitis is a symptom of various diseases. The possible complications therefore depend on the underlying disease. Often retinitis is even asymptomatic. In severe cases, however, it can lead to blindness. The basic diseases can be hereditary or acquired.
Acquired forms of retinitis are not infrequently caused by infections or autoimmune diseases. Certain types of retinitis can lead to a lot of small bleeding in the retina. Diabetics in particular are at greater risk of developing haemorrhagic retinitis (retinal bleeding). A choroidal inflammation is often associated with retinitis and is characterized by water retention in the tissue, small bleeding in the retina, and retinal detachment.
Retinitis also develops in the context of the so-called Vogt-Koyanagi-Harada syndrome. This is a disease that is directed against the body's own melanocytes due to an autoimmune reaction. This form of retinitis is associated with meningitis, pigment disorders, hair loss and an increased sensitivity to high pitched sounds. Vogt-Koyanagi-Harada syndrome leads to death in ten percent of cases.
Sometimes, with the various forms of retinitis, vision can still be severely impaired after the inflammation has healed. This is especially the case when scarring has formed on the cornea. These can lead to ulcers and small tears, which then form the basis for severe visual problems.
When should you go to the doctor?
Since retinitis does not heal on its own, this disease must definitely be examined and treated by a doctor. Only a medical examination can prevent further complications. A doctor should be consulted in the case of retinitis if the person concerned suffers from significant swelling in the area of the eyes. If the swelling does not go away on its own, a doctor should always be consulted. This can also disturb the affected person's field of vision. Since this condition is inflammation, it can also be accompanied by a fever.
Usually, retinitis is treated by an ophthalmologist. There are no particular complications and the course of the disease is usually positive. The patient's life expectancy is also not restricted by the disease. However, in the worst case scenario, if the retinitis is not treated, the affected person can lose vision completely.
Treatment & Therapy
In preparation for treatment and therapy, the specialist will determine possible risk factors in an intensive anamnesis discussion. Information about current illnesses, infectious processes or genetic hereditary diseases within the family is urgently required for the further course of treatment. Depending on the causal disease, individual therapy is carried out.
If the retinitis is caused by bacteria, antibiotics are used. This is the case, for example, with the involvement of an inflammation of the choroid (chorioretinitis). Here, eye drops containing antibiotics are usually administered. Antivirals help with a viral infection.
In rare cases, after the inflammation has subsided, scarring forms on the cornea of the eye. This leads to the formation of ulcers or small tears in the cornea, which are initially barely noticeable, but later cause enormous visual problems. An amniotic membrane (tissue obtained from the placenta) is sutured onto the affected area through a surgical procedure.
This acts like an anti-inflammatory protective layer and at the same time supports the healing of the eye with certain wound healing substances. The procedure, which only takes a few minutes, is performed under local anesthesia. As soon as the cracks under the protective membrane have healed, the amniotic membrane is removed again.
You can find your medication here
➔ Medicines for visual disturbances and eye complaintsprevention
Retinitis often occurs at a late stage as a result of infectious diseases or other health problems. Therefore, retinal inflammation cannot be prevented. However, the immune system can be strengthened to fight off viruses and bacteria.
General measures include a healthy lifestyle with a balanced diet, sporting activities, being outdoors and appropriate rest periods. However, if there are any abnormalities in the eye with pain and redness, medical advice must be sought as soon as possible. Regardless of this, regular check-ups at the ophthalmologist protect against unpleasant surprises.
Aftercare
The primary goal of retinitis follow-up is to maintain eyesight. A progressive detachment of the retina as well as a rapid destruction of the photoreceptor cells should be slowed down as they would lead to blindness in the long term. About half of the patients also develop an opacified lens (cataract) during the course. Here too, preventive measures can be taken in the course of aftercare.
The disease is hereditary, there is currently no healing method. If the diagnosis is made in adolescence, the treatment options are even greater than at a later point in time. During follow-up treatment, the ophthalmologist must consider the patient's current condition.
Some of those affected are almost symptom-free. Other sick people, in whom the retinitis is already well advanced, are already severely restricted in their vision. At this stage, not only the rods but also the cones of the retina are affected. Depending on the severity of the symptoms, the patients are treated during follow-up care.
If the symptoms of retinitis are emotionally stressful for the patient, psychotherapeutic support is also recommended. In doing so, possibilities are worked out how the person affected can cope with everyday life more easily despite the visual impairment. The development of depression is also treated preventively in the therapy sessions.
You can do that yourself
The cause of retinitis cannot yet be treated. The only effective therapy is to slow the course of the disease and relieve the symptoms.
Those affected can improve their quality of life by consulting the ophthalmologist closely and having their special glasses adjusted regularly. Special edge filter glasses with UV protection provide additional protection for the eyes. Orientation and mobility training can be used to accompany this. In this context, those affected learn how to move and orientate themselves with impaired vision. Individual complications such as cataracts or cell disorders of the macula lutea must be treated individually.
In everyday life, those affected should also ensure sufficient rest and relaxation. Retinitis is a major psychological burden that can significantly reduce the quality of life. It is all the more important to compensate for this loss with a full life. Those affected have to make use of the regular follow-up checks by the doctor and, moreover, get in touch with various specialists, as new treatment options for retinitis pigmentosa are constantly being developed, which could be suitable for patients with the necessary basic requirements.




.jpg)