One type of bacteria has made a name for itself like no other type of bacteria in the treatment of diseases and resistance to antibiotics: the Staphylococcus aureus. This germ can be found on the mucous membranes of most people for their entire life as a harmless skin colonist. But when a weakened immune system and many antibiotic therapies experienced from this germ come together, this bacterium can become a challenge to the limits of medicine.
What is Staphylococcus aureus?
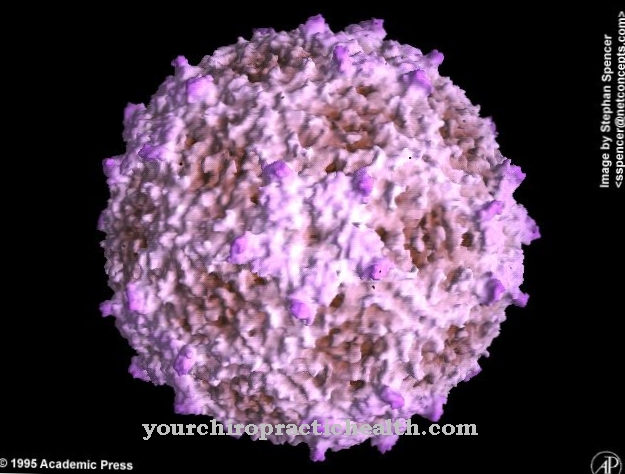
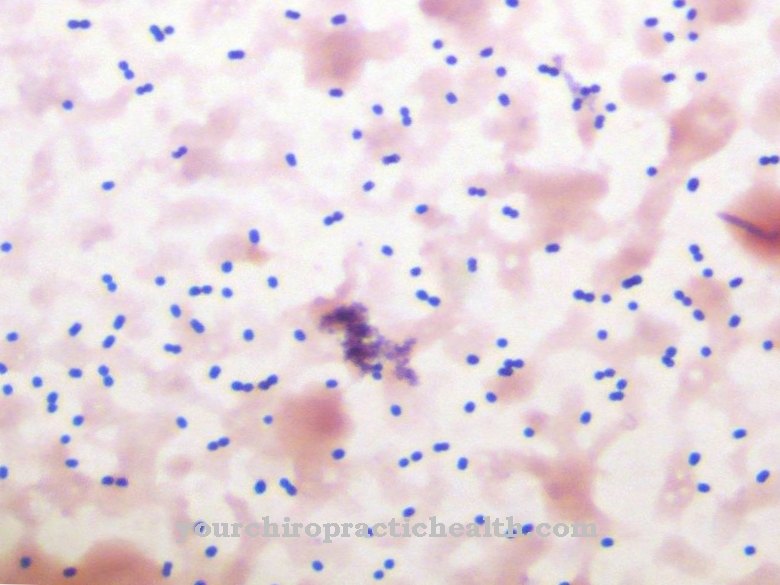
The bacterium Staphylococcus aureus Under the microscope, a spherical bacterium with a thick cell wall that can be stained in the Gram test can be seen. Often arranged in a grape shape, this bacterium is known to rarely move actively and not form spores to better survive harsh external conditions.
It measures almost a micrometer in length and can be found almost everywhere in nature, on the skin surface of humans and in the upper respiratory tract in more than three quarters of all people. Under normal conditions, this bacterium alone cannot trigger any symptoms of the disease.
Unnoticed, the Staphylococcus aureus, together with other bacteria, forms a protective screen on the human skin and has the function of not leaving any space for dangerous strains of bacteria to settle on the skin.
Meaning & function
This protective shield from bacteria is one of the most important systems for defense against pathogens in the human body. In most cases, the human body's defense system can defend itself against all kinds of pathogens.
Most possible pathogens, however, are warded off by the natural protective barriers on human skin. Without a functioning skin as a protective cover against the bacteria, the body's defense system would not be able to successfully defend itself against an invasion of bacteria of all kinds. The skin surface is one of the most important components of the defense system against pathogens.
If the skin is washed too heavily or even thoroughly disinfected, this protective film can be thinned out too much by bacteria. As a result, other types of bacteria can then settle on the skin and enter the body more easily, causing serious illness.
Even in hostile environmental conditions, the Staphylococcus aureus stay alive for long periods of time. Only temperatures above 60 degrees Celsius are sufficient to kill the Staphylococcus aureus. In a dry environment, the bacterium often survives for several months. Due to its ability to survive in acidic environments, this pathogen can also survive passage through the stomach. It is primarily these properties of survival in adverse environments that make this Staphylococcus aureus a bacterium that is widespread in hospitals.
Diseases
In most cases, the Staphylococcus aureus do not trigger any signs of illness. This bacterium can colonize the mucous membranes and the skin for a lifetime without being noticeable to humans.
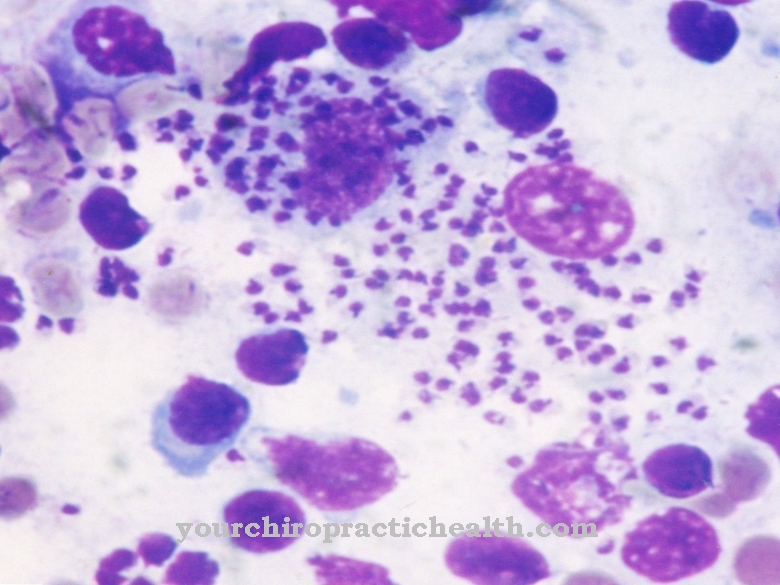
If the germ has an opportunity to enter the body directly, this germ can lead to certain diseases. This can be the case with a weakened immune defense, diabetes, damage to the skin such as psoriasis or neurodermatitis or skin injuries such as accidents, operations or the insertion of catheters.
In these cases, Staphylococcus aureus can often cause skin inflammation such as boils and carbuncles or muscle diseases such as pyomyositis. In some cases, however, the bacterium can also cause life-threatening diseases such as blood poisoning, pneumonia, toxic syndrome (TTS) or endocarditis.
Because of the bacterium's long survival time, Staphylococcus aureus can develop resistance quickly. If the germ has acquired several resistances, these germs are particularly difficult to treat because they are less sensitive to antibiotics. However, these few antibiotics can often have an unfavorable profile of action.



.jpg)


















.jpg)


