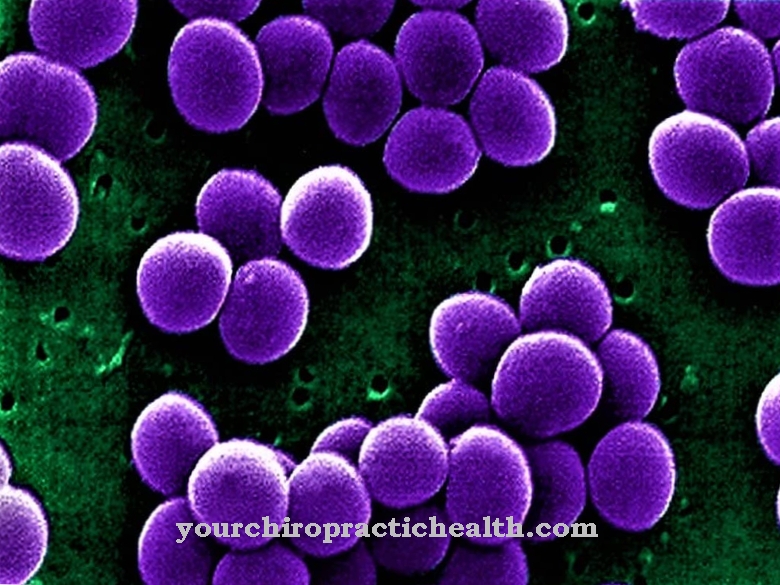
Of the Streptococcus mutans is a gram-positive, immobile, facultative anaerobic pathogen of the genus streptococci. These are spherical bacteria that usually accumulate in chain form. S. mutans occurs as a commensal in the oral cavity and is largely responsible for the development of caries.
What is Streptococcus Mutans?
Streptococcus mutans belong to the group of gram-positive spheroidal bacteria which are found physiologically in the oral flora of almost all people. These grow under facultative anaerobic conditions, which means they can multiply in the presence of oxygen, but also in its absence. Streptococcus mutans, like other streptococci, are referred to as such because they line up like a chain (Greek streptos = necklace). Streptococci are both catalase negative and oxidase negative.
What is special about the streptococci is their different hemolysis behavior on blood agar soils. These can be divided into three groups: S. mutans shows an α-hemolysing behavior, which means that they can only partially break down the hemoglobin in the agar to a product similar to biliverdin. The result is a greenish-looking edge zone around the colony, which is why S. mutans and other streptococci (such as S. bovis or S. mitis) are referred to as greening streptococci. In the case of β-hemolysis behavior, the hemoglobin is completely broken down into bilirubin, while γ-hemolysis is a misleading term, since there is no hemolysis at all.
Occurrence, Distribution & Properties
Streptococcus mutans belongs to the normal flora of the human oral cavity and is present in almost everyone. The parents are usually responsible for the first contact with the S. mutans on the baby, for example by putting the baby's spoon or pacifier in the mouth, where the bacterium can be found in abundance. In addition, numerous microorganisms are transmitted through kissing.
However, the presence of S. mutans is not to be equated with the development of caries. The bacterium must first be given the appropriate conditions by consuming a lot of sugary foods and drinks. Only then can the bacterium generate the acidic environment that attacks the tooth enamel. The number of S. mutans correlates with the risk of developing caries in a patient, i.e. the more bacteria there are in the saliva, the higher the probability of developing caries.
The S. mutans and other streptococci have hemolysin. This enables them to destroy the erythrocytes on the blood agar, which results in the typical α-hemolytic behavior, which is characterized by the fact that the colonies on a blood agar are surrounded by a greenish shimmering halo.
In addition, S. mutans has other virulence factors that are related to caries formation. The pathogen can form glucan polymers from sucrose, a sugar found in the chyme, which are produced by glucosyltransferases. This enables the bacterium to attach itself to the tooth enamel and thus develop firm adherence. In addition, the S. mutans can ferment the carbohydrates in the food to lactate (lactic acid). The lactic acid forms the acidic environment that attacks the tooth enamel and thus leads to the demineralization of the substance.
Since the S. mutans is able to excrete acids, it must also be able to survive in this environment, so the pathogen has developed a certain acid resistance in order to protect itself from decomposition by the lactic acid.
In addition to protecting against acid, S. mutans also protects against human immune defenses. Antibodies of the immunoglobulin A (IgA) type are mainly found in saliva. S. mutans forms a so-called IgA protease, which deactivates these antibodies and can thus weaken the immune system.
Furthermore, the S. mutans can compete with other bacteria for food. In order to gain this, S. mutans forms bacteriocins with which foreign bacteria can be attacked.
You can find your medication here
➔ Medication for toothacheIllnesses & ailments
Streptococcus mutans is the main causative agent of tooth decay, which is one of the most common diseases worldwide. Caries in itself is not contagious, but the pathogen can be transmitted. Usually the teeth are surrounded by a biofilm that is full of bacteria, including S. mutans.However, if the tooth is exposed to some risk factors, the likelihood increases that the bacteria will ferment carbohydrates from food and form lactic acid, which attacks the tooth and thus leads to tooth decay.
Such risk factors are, for example, the number of S. mutans, poor dental hygiene or sugary foods. The dentist divides tooth decay into different stages, depending on how deep the bacteria has penetrated the tooth. If the tooth has a filling, it can loosen and peel off. In addition, patients usually complain of an unpleasant taste or bad breath.
If the pathogen penetrates close to the pulp (tooth pulp), toxins formed can be released and cause inflammation. The sensitivity of the nerve fibers is increased and the patient has an increased feeling of cold or warmth. In addition, there is a strong feeling of pain, which can be permanent or recurring. If the pathogen gets all the way into the pulp, an abscess can form, the tooth can die and must be removed.





















.jpg)


