The Synovitis is a painful phenomenon that can occur especially in old age or with long-term stress. Synovitis is particularly noticeable when tendons, joints or muscles are impaired or are permanently stressed without regeneration phases.
What is synovitis?

© joshya - stock.adobe.com
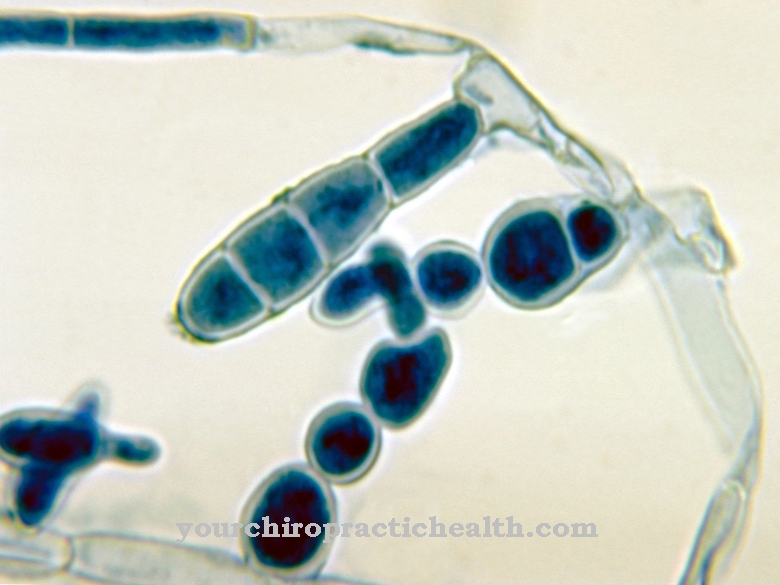
The medic referred to as Synovitis (or Synovitis) an inflammation of the mucous membranes that line the tendon sheaths, joints and bursa from the inside.The mucous membrane produces a certain amount of fluid, which ensures that the movement between the bony structures is free of friction.
Due to a permanent pressure load, which is given during work or also in the context of sporting activity (kneeling positions are beneficial), inflammation of the mucous membrane can develop. The inflammation can also spread to the connective tissue and bony structures; as part of this expansion, acute synovitis can mutate into chronic synovitis.
causes
Especially people who mainly kneel down (such as cleaning staff or tilers) are mainly affected by synovitis. Occasionally, athletes also complain of corresponding complaints, with synovitis often taking a chronic course. The chronic course of synovitis occurs when there is no recovery in the context of acute forms and training continues or the joints that cause pain are not spared.
Older people, whose regenerative abilities are already limited and sometimes already have a higher degree of wear and tear on their joints, usually suffer from synovitis. The painful synovitis also occurs with other inflammatory diseases, so that synovitis and arthritis, which are sometimes responsible for the symptoms, are diagnosed.
Symptoms, ailments & signs
The person concerned complains after an excessive strain (for example, if he overexerted himself in the context of physical activity or took part in a sporting competition) mainly about an increasingly intense pain. The pain occurs in combination with restricted mobility.
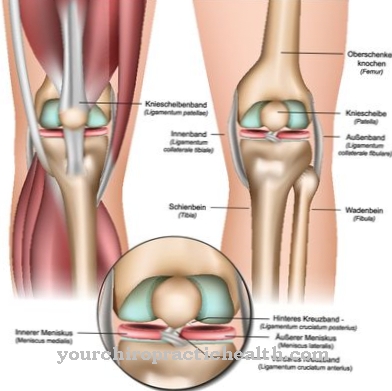
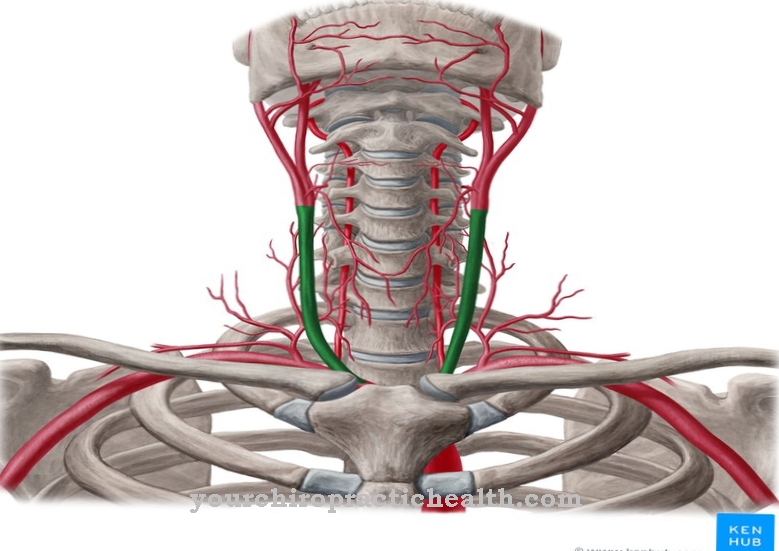
Sometimes the affected limb can swell; as a result, the area causing the pain becomes reddened. Those symptoms arise due to the inflamed mucous membrane, as an increased blood flow is activated here. In the context of synovitis, fluid accumulations occur in the relevant joints or joint capsules (e.g. in the knee joint), which are subsequently responsible for restricting movement.
Diagnosis & course of disease
The doctor diagnoses synovitis when other inflammatory diseases, such as arthritis, can be completely ruled out. For this reason, different examinations are usually carried out to confirm the diagnosis of synovitis on the one hand and to exclude diagnoses such as arthritis on the other.
The problem is that - especially in old age - several diseases can trigger the classic symptoms of synovitis. Thus, of course, there is also the possibility that synovitis will go undetected. Even at the beginning, the synovitis expresses itself as a "rubbing sensation"; the patient “waits” for the pressure to be released but notices that the joint continues to “rub”. As a result, pain, redness and swelling increase.
The doctor examines the affected joint. To do this, he uses the ultrasound device. The doctor can use ultrasound to determine whether synovitis is suspected. The course of the disease is mainly influenced by the activity of the person concerned. In particular, tilers and cleaners, who mainly crouch or kneel, are at risk of synovitis becoming so bad that even the articular cartilage is destroyed and, as a result, the bones are attacked.
Complications
Synovitis usually occurs in combination with restricted mobility. As a result, the affected limb can swell, causing redness and further pain. Normal movement is usually no longer possible due to the accumulation of fluid in the affected joints. Further complications can occur if arthritis is diagnosed.
Then the bone density continues to decrease as the disease progresses and the chances of recovery from synovitis worsen. Under certain circumstances, chronic pain develops, combined with a decrease in the quality of life and performance of the person concerned. This can lead to depressive moods and other psychological ailments that must be treated separately. Surgical intervention can cause bleeding, bleeding, and infection in the affected area.
Nerve injuries, which can be associated with temporary impairment of movement and sensitivity disorders, rarely occur. The surgery can also lead to further irritation of the affected area, which may worsen the synovitis. Prescribed painkillers can cause side effects and interactions and trigger allergies. In the event of a longer illness, addictive behavior may develop and the resultant addiction.
When should you go to the doctor?
A doctor is needed if the person has persistent pain. Irregularities in the tendons, joints or muscles should be examined and treated. If, after a restful night's sleep or adequate rest and rest, the symptoms are alleviated and the patient is recovered, in most cases no doctor needs to be consulted. In these situations, it is an overload of the body, which heals automatically through the natural regeneration processes.
A doctor is required in the event of recurring, persistent or increasing health problems. If there is only a slight improvement in wellbeing after a regeneration phase, this is not enough. Further examinations are necessary so that a diagnosis can be made by researching the cause. Restrictions in general movement sequences, a decrease in normal physical performance and irregularities in joint activity must be presented to a doctor.
Irritation, accumulation of fluids or swelling are all signs of a health problem. A sensation of warmth near the joints, an increase in heart activity, or reddening of the skin are symptoms that suggest synovitis. Since the affected person is threatened with a chronic illness if the disease progresses poorly, the symptoms should be responded to at an early stage. In cooperation with a doctor, changes in the usual movement sequences as well as optimization of resilience can be made.
Therapy & Treatment
At the beginning of treatment, it is advisable that the inflamed area of the body is immobilized and relieved. This is the only way to reduce the swelling and reduce the pressure exerted on the tissue. The patient should regularly cool the affected area with ice packs or ice; this process also ensures a reduction in swelling and pain.
Pain relievers and anti-inflammatory drugs can help relieve the acute phase of synovitis. It is important that the intake of the tablets is discussed with the family doctor or that check-ups are carried out at regular intervals to determine whether the medication is also having the desired effect.
If the symptoms do not improve or the symptoms worsen so that medication or cooling measures no longer help, the patient has to undergo an operation. The doctor decides in favor of the keyhole technology. The doctor makes a few small incisions in the affected area; the cuts are just big enough that the necessary instruments or the camera can be inserted.
With this method it is possible that any outgrowths of the mucous membrane can be treated. As a rule, surgery is the only way that synovitis can be permanently cured. In a few cases, however, a deterioration of the synovitis was found, since the regions already affected - due to the operation - were even more irritated.
You can find your medication here
➔ Medicines for joint painprevention
Synovitis can very well be prevented. Athletes can take action against synovitis with warm-up phases; Sometimes people who are at risk of developing synovitis due to their occupational activities can take precautions by swimming. Of course, it is important that enough regeneration phases are observed. If the first signs of synovitis have already been noticed, you should therefore spare the affected joints.
Aftercare
In the case of synovitis or joint mucosal inflammation, follow-up care is advisable until it has completely healed. There is acute and chronic synovitis. The follow-up treatment is adapted to the respective form of the disease. In the acute course, follow-up care ends when the symptoms subside. In the case of chronic synovitis, it is long-term.
The symptoms should be alleviated in both courses and completely eliminated in the acute form. Another goal is to prevent secondary diseases. The person affected can also counteract the symptoms by taking painkillers, protecting the inflamed joint and protecting against overload. The swelling can be accelerated by additional cooling.
If the patient has to kneel a lot due to work and the inflammation keeps returning, he should consider changing jobs. In the case of severe disease, only the surgical route remains. The excess mucous membrane is removed during the operation using a keyhole procedure.
Follow-up care depends on the postoperative condition: If the joint has subsequently been able to heal, no further follow-up care is necessary. The inflammation was eliminated. If the symptoms worsen, other healing methods must be discussed. The development of chronic synovitis should be prevented, the mobility of the joint must be restored.
You can do that yourself
In the case of acute synovitis, a doctor should be consulted immediately. The self-help measures are limited to taking care of yourself and taking the medication according to the doctor's instructions.
In chronic synovitis, the affected joints should not be subjected to any further stress. If the condition is related to rheumatoid arthritis, additional measures must be taken. The patient needs a walking aid and special care from a physiotherapist. In addition to conservative drugs, synovitis can be treated with various natural medicinal products. Pain-relieving and anti-inflammatory agents such as aloe vera or nettle extract are particularly useful to relieve joint pain. A tight bandage must be worn while the joint is immobilized. Physiotherapy includes warming compresses, electrophoresis and electromagnetic wave therapy.
After an operation on the joint, the leg must not be moved at all for three to four days. In the first few weeks, any stress should be avoided until the doctor gives his okay. Synovitis is a serious disease that can take on very different forms. That is why self-help must also be strictly monitored.


.jpg)









.jpg)




.jpg)


