At a Chest deformity it concerns malformations of the thorax or deformities of the chest wall. These malformations are either congenital or acquired. Congenital forms of thoracic deformities show up in the majority of cases in early infancy or early childhood. Other malformations of the thorax, on the other hand, only manifest themselves during puberty.
What is a chest deformity?

© SciePro - stock.adobe.com
Basically, a Chest deformity a shape of the chest wall or the rib cage that deviates from the usual norm. Corresponding malformations can occur for genetic or acquired reasons. In the majority of cases, the chest deformity is a funnel chest.In most cases, this malformation manifests itself in a sunken sternum and is the most common form of deformity.
If the rib cage is curved forward, it is referred to as a so-called keel chest. The Harrenstein deformity is a special form, in which the sternum is twisted. If the sternum structures do not completely fuse, a so-called sternum gap is created. If the embryo's rib cage does not close completely, it is a thoracic shisis.
An asymmetrical appearance of the anterior chest wall is possibly due to a so-called fork rib. This sometimes shows connections to Ehlers-Danlos syndrome or so-called chondrodysplasias, such as metaphyseal chondrodysplasia. In principle, thoracic deformities occur more frequently in connection with various syndromes.
These include, for example, Ellis-van-Creveld syndrome, funnel chest or keel chest, asphyxiating thoracic dysplasia, Marfan syndrome, homocystinuria, Poland syndrome or spondyloepiphyseal dysplasia. In addition, thoracic deformities in connection with rickets or a rachitic rosary as well as multiple pterygium syndrome and metaphyseal chondrodysplasia of the Jansen type are possible.
causes
According to the current state of medical research, the causes of the formation of thoracic deformities have not yet been fully clarified. For example, disturbances in the growth of the costal cartilage, which represent the connection between the bony ribs and the sternum, are under discussion. In examinations with the electron microscope, a faulty structure of the cartilage base substance can sometimes be seen.
Inflammatory reactions inside the cartilage were also found. As a result, certain areas of cartilage grow unchecked. These press the breastbone outwards or inwards. Existing connections to certain syndromes are also known, for example Marfan's syndrome.
The only thing that is certain so far is that the development of thoracic deformities is very complex. In numerous cases, genetic causes also play an important role in the formation of the deformities. This is the case, for example, with growth disorders on the costal cartilage. In addition to some of the syndromes already mentioned, which can occur in connection with chest deformities, corresponding malformations are also possible, for example due to tumors on the chest wall.
Symptoms, ailments & signs
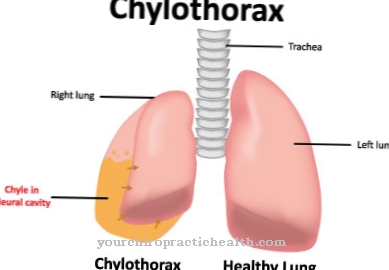
Numerous different symptoms and complaints are possible in the context of chest deformities, which differ greatly depending on the syndrome and form of the malformation. In many cases, thoracic deformities are generally associated with so-called secondary pathologies. These include, for example, compression atelectasis, reduced cardiac output, respiratory insufficiency, reduced performance, scoliosis and other poor posture.
In addition, in many cases the deformities lead to considerable psychological stress for the patient, which in certain circumstances is associated with social demarcation and isolation. As a consequence of severe chest deformities, chronic respiratory insufficiency or atelectasis can occur in some cases.
Diagnosis & course of disease
In principle, a number of examination-technical methods are available for diagnosing thoracic deformities, the use of which the attending physician decides depending on the individual case. If a patient presents himself to the specialist for the first time, a thorough anamnesis or a discussion of the medical history takes place. For example, symptoms, the course of the disease and family dispositions are clarified.
This is followed by a so-called initial measurement, an EKG examination and a test of the lung function. Together with the clinical examinations, a differentiated picture of the present form of the thoracic deformity and the potential health impairments is now possible. Because consequential damage is not to be expected in all patients.
However, there is no consensus in medical research as to whether thoracic deformities are generally associated with reduced lung function and performance as well as heart problems. In numerous cases, postural disorders are evident in the context of thoracic deformities, especially with a funnel chest or a keel chest.
The shoulders of the affected patient hang forward and there is a pronounced hollow back. In addition, there is often a so-called hunchback and a weak abdominal wall. In some cases, scoliosis of the spine shows up at the same time. In principle, the aim of clinical examinations is to identify all accompanying illnesses in order to initiate suitable measures to treat the symptoms.
Complications
A common form of chest deformity is the so-called funnel chest. While children and adolescents usually do not have to worry about major physical restrictions, complications regularly occur after puberty has ended with increasing age. The misalignment of the ribs can negatively affect the spine and lead to poor posture.
Very often kyphosis sets in, which is accompanied by bent shoulders and a protruding stomach. The unnatural curvature of the spine also puts more strain on the intervertebral discs, which can cause severe back pain. In addition, due to the narrowing of the incubator, further complaints such as shortness of breath, palpitations and rapid physical exhaustion can be expected.
If a surgical procedure to correct the funnel breast is necessary or if this is done for cosmetic reasons, a number of complications can arise. The procedure is minimally invasive, but is still carried out under general anesthesia, which is generally associated with certain risks, in particular serious circulatory problems up to and including circulatory collapse.
The patient may also be allergic to the metal introduced for correction. If premature removal becomes necessary for this reason, this can weaken or even negate the effect of the operation. Serious complications such as organ injuries, especially to the heart or lungs, are very rare, but cannot be completely ruled out.
When should you go to the doctor?
A congenital chest deformity is usually diagnosed immediately after childbirth. A birth is accompanied by midwives, doctors or nurses. The newborn is examined intensively by the obstetrician team immediately after it is born. During this initial examination, irregularities in the body structure are already detected. The newborn is presented to the pediatrician for further examinations and to clarify the cause. Parents and relatives do not have to take action independently in these cases. The necessary measures are completely taken over by the nursing staff present.
In the case of an acquired chest deformity, there is a triggering event. A fall, an accident or an act of violence can be the reason for the deformation. If there are changes in the body structure and in particular in the chest, a doctor must be consulted.
If bulges in the chest wall or rib cage are found during the growth and development process of a child or adolescent, a doctor should be consulted. Impairment of breathing, pain or restricted mobility are further signs of an irregularity. They need to be examined and treated.
Consult a doctor in the event of impaired physical performance, irregularities in the heart rhythm and changes in the appearance of the skin. Poor posture of the upper body, disorders of the muscular system and psychological problems should also be presented to a doctor for assessment. A diagnosis is necessary so that a treatment plan can be worked out.
Treatment & Therapy
In the case of thoracic deformities, the therapeutic measures are primarily based on the type of disease present. Both conservative physiotherapeutic treatment approaches with targeted exercises and surgical operations are possible. In addition, the deformity should be checked by a doctor at regular intervals. A funnel breast can be treated with a suction cup to lift the front chest wall.
prevention
Concrete measures to prevent chest deformities are not yet known. Basically, it is important to maintain a healthy posture and sufficient exercise in order to prevent postural damage.
Aftercare
In the case of thoracic deformity, direct follow-up care measures are in most cases severely limited, so that those affected depend on immediate medical treatment for this disease. The earlier the disease is recognized and treated, the better the further course will usually be. In most cases, self-healing cannot occur, so that a doctor should be consulted at the first signs of the disease.
Most patients with this disease also need various cosmetic interventions that can alleviate and limit the symptoms. This may have to be repeated more often, so that a complete limitation of the disease is not possible. Most of those affected are also dependent on the support of their own family or their partner, which can also prevent depression or other psychological disorders.
The chest deformity does not reduce the life expectancy of the person affected. Further follow-up measures are not necessary and usually not possible. Contact with other affected parties to exchange experiences can be useful.
You can do that yourself
Patients with a chest deformity often suffer from various complaints that result from the deformity of the chest. Therefore, the quality of life of those affected is partially limited. If it is a congenital chest deformity, those affected learn to deal with the disease early on. The situation is often more difficult for those patients who only acquired the disease later in life.
In some cases, the chest deformity is associated with reduced performance because the cardiac output is reduced. Self-help measures can support medical therapy for this type of complaint, but in no way replace it.
Patients visit their doctor for regular check-ups and take part in physiotherapy. Since poor posture can also arise from the chest deformity, regular physiotherapeutic training is particularly important. Patients with thoracic deformity can continue the exercises they have learned at home.
Social problems and bullying can cause difficulties, as the patients deviate more or less from the norm due to the chest deformity and thus attract attention. Participation in self-help groups and social exchange with other sick people are ways to reduce these stress factors. In this way, patients can expand their circle of acquaintances and thereby reduce social stress.



.jpg)