In the Tularemia it is a highly contagious infection that occurs very rarely in Germany and that can be transmitted to humans by mammals. Due to the plague-like course and the predominant occurrence in wild rabbits and hares, one also speaks of the Rabbit plague.
What is tularemia?
Tularemia is triggered by the bacterium Francisella tularensis, so it is a bacterial infection. Since the disease can be transmitted from small mammals to humans, it is called a zoonosis.
The disease is very rare in Germany, with the predominant occurrence in northeastern Europe, Asia and North America. Depending on the entry point of the pathogen, different manifestations of tularemia occur. The clinical picture can differ depending on the entry point of the pathogen, some examples are:
Ulceroglandular Tularemia: Ulceration at the point of entry and sudden fever
Glandular tularemia: Swelling of the lymph nodes
Abdominal tularemia: Typhoid-like clinical picture, spleen and liver swell, diarrhea and pain in the abdominal area (organs of the abdominal cavity are affected)
Intestinal tularemia: Abdominal pain and diarrhea, vomiting and nausea
causes
The cause of the Tularemia is based on a bacterial infection with Francisella tularensis. Ticks, fleas and lice can serve as a reservoir for the bacterium, and it is also able to survive in frozen rabbit meat for up to three years.
The parasites that carry the pathogen can transmit the bacterium to both humans and mammals through a bite. Other ways of infection with tularemia come about through contact with infected mammals. This contact can take the form of bites or scratches from infected animals; it is also possible to pick up the pathogen through direct contact with excretions or blood from infected animals.
In order to become infected with tularemia, however, no direct contact is necessary; the causative agent of tularemia can also be ingested through the air or contaminated water.
Symptoms, ailments & signs
The rabbit plague causes different symptoms in animals and humans. The eponymous rodents usually develop septicemia a few days after infection, which spreads throughout the body. The affected animals show typical side effects of fever, an increased respiratory rate and enlarged lymph nodes and an enlarged spleen.
In addition, the animals appear severely weakened. Most of the rodents die of blood poisoning about two weeks after infection. Infected dogs do not usually die of rabbit plague, but they can develop distemper-like symptoms after infection. In humans, an infection with the Francisella tularensis bacterium is usually associated with symptoms that are similar to a flu-like infection.
The patients initially suffer from a fever and headache. Often these symptoms are accompanied by nausea and vomiting. Many people also have swelling of the lymph nodes where the bacterium entered the body. If the infection is not recognized and treated with antibiotics, a life-threatening condition can develop.
This is often announced by severe chills and abdominal pain. Many patients also develop severe inflammation of the throat. In humans, rabbit plague is not associated with symptoms that are specific to this disease, which is why it can only be determined beyond doubt by a blood analysis.
Diagnosis & course
The diagnosis of the Tularemia can often not be clearly identified and in some cases does not even occur, as the course of the disease sometimes resembles that of a flu-like infection.
However, based on the frequently occurring symptoms, such as ulceration of the skin and swelling of the lymph nodes, conclusions can be drawn about tularemia. However, a direct diagnosis is only possible by means of animal experiments. For this purpose, a blood sample is taken and injected into a test animal. If the pathogen is present, this can be demonstrated on the basis of the antibody formation of the test animal, but it should be noted here that due to the similarity of the tularemia to the thymus pathogen, a wrong diagnosis can be made.
In humans, the incubation period is 1-10 days, after which the typical symptoms appear. If tularemia is detected early and treated appropriately with antibiotics, there are hardly any complications, but if the disease remains untreated, it leads to death in 30% of all cases. Once the disease is over, there is lifelong immunity to the tularemia pathogen.
Complications
In the absence of or inadequate treatment, tularemia can cause a variety of symptoms that can lead to serious complications. Typical of rabbit plague is the noticeable swelling of the lymph nodes at the infection site, which is occasionally associated with fever and a general feeling of illness. If it is severe, the fever rises to over 40 degrees Celsius and causes cardiovascular complaints, dehydration and other complications.
Some patients also suffer from abdominal pain and migraines, both of which are associated with severe malaise and a decrease in quality of life. The characteristic inflammation of the throat can spread and possibly cause inflammation of the sinuses or even pneumonia. The rabbit plague also promotes the development of sores on the skin, which can also become infected or cause bleeding and scars.
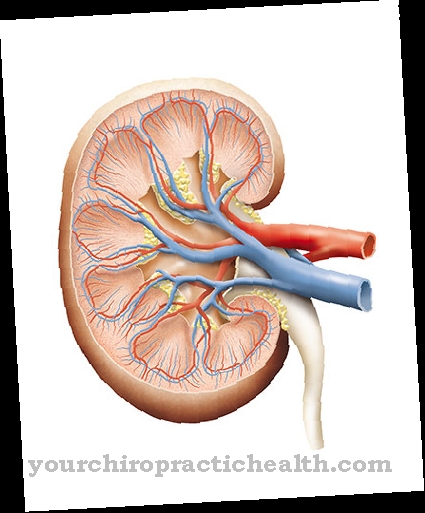
Drug treatment using antibiotics such as doxycline or gentamycin is sometimes associated with side effects and interactions. Above all, gastrointestinal complaints are problematic, as these correlate with the symptoms of tularemia and can thus cause severe pain and fever. Long-term use of the corresponding preparations can severely damage the internal organs, especially the liver, kidneys and heart.
When should you go to the doctor?
In the case of tularemia, the person affected is dependent on a medical examination and treatment in any case, as this cannot lead to an independent healing. The earlier the disease is recognized, the better the further course is usually. In the worst case, tularemia can even lead to the death of the person affected, so that a doctor should be contacted as soon as the first symptoms and signs of the disease appear. A doctor should be consulted in the case of tularemia if the person concerned suffers from an increased respiratory rate and if the patient's spleen is significantly enlarged.
The symptoms of common flu can also indicate this illness. Most patients have severe pain in the abdomen and an inflammation in the throat or throat. If the symptoms of the flu do not go away after a few days, you should definitely consult a doctor. For tularemia, either a general practitioner or a hospital can be visited.
Treatment & Therapy
A treatment of Tularemia happens with an antibiotic, this can be doxycline, ciprofloxacin or gentamycin, the greatest successes being recorded with streptomycin. Sulphonamides and penicillin should be avoided because the pathogen is resistant to them. The antibiotic of choice should be taken for 10-17 days to ensure a relapse and complete recovery from the tularemia.
prevention
Against Tularemia A vaccine already exists, but it is not available on the German market. Prevention of tularemia is also possible by following simple rules of conduct.
When coming into contact with wild animals, one should always wear disposable gloves and avoid handling suspicious animals entirely. In addition, dust-proof breathing masks should be worn when processing wild animals, including skinning and gutting. Veterinarians, forest workers and hunters represent particular risk groups.
Aftercare
In tularemia (rabbit plague), the extent of follow-up care is determined by the type of pathogen and the severity of the disease. Tularemia pathogens can essentially be of the subtype "F. tularensis ”and the subtype“ holarctica ”. The subtype "F. tularensis ”is common in North America. In 30 to 60 percent of all untreated cases of illness, the pathogen leads to the death of the sick person.
In the event of death, follow-up care focuses on coping with grief. For relatives of the first degree, psychological counseling or care is recommended. The “holarctica” subtype occurs almost exclusively in Europe. The probability of dying from tularemia caused by the “holarctica” subtype tends towards zero.
Therapy for tularemia is used in both the “F. tularensis ”as well as with the“ holarctica ”subtype basically started with clinical medication (ciprofloxacin as monotherapy). After the clinical stay, drug therapy is continued for about 14 days during follow-up care. In order to check the success of the therapy, blood analyzes are also planned in the follow-up.
Often the "holarctica" subtype even heals spontaneously. With the subtype "F. tularensis ”, on the other hand, a severe course of the disease can be expected on a regular basis. Secondary symptoms such as endocarditis, severe septicemia, pneumonia and liver and kidney failure can occur here. In addition to continuing the drug therapy, the focus of the follow-up care is then on treating the symptoms.
You can do that yourself
Tularemia is treated with antibiotics such as streptomycin or gentamicin. The medication must be taken strictly according to the doctor's instructions. It is also important to initiate therapy early in order to avoid a serious course of the disease.
Medical treatment can be supported by bed rest and an appropriate diet. The weakened body needs sufficient fluids and nutrients, especially in the acute phase of the disease. Later, light foods should be consumed so as not to put any further strain on the irritated gastrointestinal tract. Because the condition can lead to conjunctival discomfort, you are not allowed to drive. Operating heavy machinery is also prohibited. In the case of external inflammation or ulcers, care products from the pharmacy can help. In consultation with the doctor, ointments made from natural substances can be tried.
Pregnant women who have been diagnosed with rabbit plague should contact a specialist clinic. Since the use of strong antibiotics is not permitted during pregnancy, alternative treatment methods must be chosen.
Basically, with rabbit plague, rest and rest, in conjunction with following medical guidelines. Affected people can exchange ideas with other sick people in internet forums or in a specialist center. The support of the partner or another caregiver is also important.