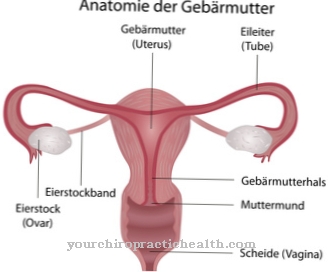
At a Uterine prolapse it is a prolapse of the uterus. The uterus slips through the birth canal.
What is a uterine prolapse?
Of the Uterine prolapse (Prolapse of the uterus) is classified as the worst form of uterine subsidence (Descensus uteri). This results in the uterus (uterus) being pushed through the birth canal. This in turn everts the vagina and emerges outside the body. The reason for this is that the retaining straps give way.
The woman's uterus is a muscular organ. It is fixed by ligaments and muscles within the pelvis. If these ligaments and muscles weaken and stretch, they are no longer able to secure the uterus in place. The consequence of this is a prolapse. This shows up when the uterus is lowered or when it slips out of its normal position.
A uterine prolapse occurs either partially or completely. In a full incident, the uterus will slide off in such a way that part of it can be seen outside the vagina.
causes
Prolapse of the uterus is caused by the same reasons that cause lowering of the uterus. This is a weakness of the connective tissue that is congenital or acquired at birth. Certain risk factors increase the risk of uterine prolapse. Increasing age is considered a high risk factor, which leads to a lowering of the estrogen level in the body.
Estrogen is important for strong pelvic floor muscles. The risk of uterine prolapse is also high in women who have had multiple vaginal births. So pelvic tissue and muscles can be negatively affected by the birth process. The risk of an incident after the menopause is particularly pronounced.
In addition, activities that put pressure on the pelvic floor muscles have a positive effect on uterine prolapse. Injuries during the birth process, chronic constipation, persistent cough and obesity are classified as further risk factors.
Symptoms, ailments & signs
The symptoms of uterine prolapse depend on the extent of it. If there is just a minor incident, there may be no complaints at all. If, on the other hand, the prolapse is moderate or severe, vaginal bleeding, excessive discharge, constipation, repeated inflammation of the urinary bladder or a pulling sensation in the pelvic region can occur.
In addition, the women affected feel as if they are sitting on a ball. They also have difficulty having sexual intercourse. It is not uncommon for the cervix to protrude from the vagina. In rare cases, there is also a risk of total prolapse. The entire uterus emerges from the entrance of the vagina and turns inside out. If you experience symptoms like this, you should see a doctor as soon as possible.
Diagnosis & course of disease
If there is a suspicion of a sagging uterus or a uterine prolapse, the attending gynecologist will first check the patient's medical history. It is not uncommon for the suspicion of an incident to be confirmed by the statements of those affected. Following the questioning, the gynecologist conducts a gynecological examination during which, among other things, he inserts a speculum into the vagina.
With the help of this instrument, he checks the uterus and the birth canal. As a rule, the examination takes place while lying down. If necessary, the patient must also get up. To determine the degree of severity of the uterine prolapse, the patient performs pressure movements as when defecating. It depends on the severity of the finding whether further examinations are necessary.
This can be a sonography (ultrasound examination) of the kidneys. It is used to rule out urine congestion. Medical treatment for uterine prolapse is not always necessary. In severe cases, however, the prolapse of the uterus can adversely affect the functions of the bladder and bowel. Disorders of the sexual functions are also possible.
Complications
In most cases, the complications and symptoms of uterine prolapse depend very much on the exact severity of the disease. For this reason, a general forecast is usually not possible. Those affected suffer from profuse vaginal bleeding and thus also from pain. Constipation or various inflammations and infections can also occur and have a very negative effect on everyday life.
The urinary bladder in particular can be damaged as a result, so that the patients also suffer from pain when urinating. The uterine prolapse can also cause discomfort or pain during sexual intercourse. This has a negative effect on the relationship with one's own partner and can lead to complications. The earlier the disease is diagnosed, the higher the probability of a positive course of the disease.
Treatment is usually not associated with further complications. The symptoms can be alleviated with the help of medication and pelvic floor exercises. In some cases, the uterus is removed through surgery. Since this distance can also lead to psychological complaints, many sufferers and their partners are dependent on psychological treatment.
When should you go to the doctor?
A doctor is needed if there are problems with the female genital organs in women or sexually mature girls. If there are discomforts in the abdomen, if there are impairments during the sexual act or if there is a feeling of tightness in the vagina, the irregularities should be examined. Sexual apathy or malaise during intercourse are signs of a health disorder. If there are no accompanying circumstances that can be explained, a doctor should be consulted to establish the diagnosis. Discrepancies in the monthly cycle, a foreign body sensation in the abdomen or sudden malaise must be clarified by a doctor.
Uterine prolapse is characterized by unexpected abnormalities in the genital area. The symptoms can be perceived without a significant incident while moving, changing clothes or using the toilet. Since no spontaneous healing is to be expected, a medical consultation should take place. Sudden bleeding, unusual vaginal discharge, or sensory disturbances around the uterus are other indications that should be investigated.
Patients often complain of a pulling sensation in the abdomen, which does not correspond to the time of menstrual bleeding. A doctor is needed to clarify the cause and draw up a treatment plan. If tissue at the exit of the vagina can be felt with the fingers, action is required. To avoid complications, a doctor should be seen immediately.
Therapy & Treatment
Treatment of uterine prolapse is possible in both a conservative and an operative way. Conservative measures include a. an estrogen replacement therapy, the relief of the pelvic structures by reducing body weight and a special training of the pelvic floor. These include, for example, Kegel exercises, which are used to strengthen the muscles of the vagina.
Another therapy option is the insertion of a pessary into the vagina. This prevents the organs from sinking further. The cube-shaped or ring-shaped instruments are made of silicone or soft rubber. However, they are used less frequently nowadays because they can create pressure points in the vagina. They also need to be replaced regularly.
If there is a serious uterine prolapse or if there are pronounced side effects such as urinary incontinence, surgery is usually necessary. This serves to restore the holding apparatus of the genital organs and the pelvic floor. The surgeon tightens the organs and brings them back to their original position.
Which surgical procedure is used depends on the extent of the prolapse and the age of the patient. In addition, possible wishes for children play a role. In some cases, the complete removal of the uterus can also be useful, which is done as part of a hysterectomy. The procedure takes place either through the abdomen or through the vagina. If the patient would like to have children, the doctors advise against an operation. Childbirth often renders the results of an intervention ineffective again.
prevention
A healthy body weight is recommended to prevent uterine prolapse. Furthermore, regular Kegel exercises should be done to strengthen the pelvic floor muscles.
Aftercare
Follow-up treatment is important if uterine prolapse is treated surgically. Usually the patient has to stay in the hospital for three to five days. The length of the hospital stay also depends on your general state of health.
If there are no difficulties urinating and there are no other problems, the patient will be discharged and allowed to continue to recover in her own four walls. For uncomplicated healing of the operated body region, however, consistent rest is necessary in the first two weeks after the procedure. If there is still pain after the operation, this is usually treated with light pain medication.
Aftercare also includes avoiding bending down, lifting heavy objects or standing for long periods. The same applies to strenuous shopping. Therefore, it is advisable to seek appropriate help from loved ones or friends. Sports activities must also be avoided in the first two weeks after the operation.
However, regular walks that stimulate digestion are useful. A digestive diet is also recommended. This can counteract strong pressing when visiting the toilet. In some cases, the regulation of bowel movements must be stimulated by taking appropriate drugs.
After the operation, the patient must not have sexual intercourse for about six weeks. A fortnight after the operation, however, she can start doing light exercise again. These include gymnastics or yoga.
You can do that yourself
If signs of uterine prolapse are noticed, a doctor should be consulted. A lowering of the uterus is not necessarily a medical emergency, but it must be clarified medically. If the symptoms cause problems, medical advice is required.
Pelvic floor training can be used to accompany medical diagnosis and therapy. Regular workouts with the exercise ball or other aids strengthen the pelvic floor and prevent the uterus from slipping further. If the uterus has already subsided, this cannot be reversed through training. However, pelvic floor training prevents secondary symptoms such as incontinence. Women who have been diagnosed with uterine prolapse often feel unattractive and uncomfortable in their bodies. Targeted pelvic floor training helps to improve self-esteem.
Conversations with other affected women also help. It is even more important to talk to the partner about the problem. The gynecologist can provide information about alternative options. For example, it is possible to use a so-called pessary, which supports the vagina or uterus and prevents further lowering. Finally, it is important to accept the physical changes as a natural part of childbirth and aging.


.jpg)














.jpg)