The air flow into the lungs and air flow out of the lungs are covered by the term ventilation or ventilation combined. The ventilation is used for gas exchange in the lungs, the alveoli give off molecular oxygen to the blood and mainly take up carbon dioxide from the blood. The ingested gaseous carbon dioxide is exhaled from the lungs with the air flow and released into the environment.
What is the ventilation?

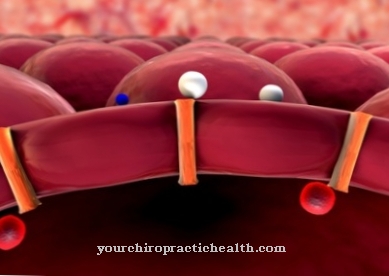
The term ventilation is used to summarize the inflow of air into the lungs and the outflow of air out of the lungs. The necessary gas exchange takes place in the alveoli. Part of the inhaled molecular oxygen is absorbed and dissolved by the carbon dioxide-rich blood in the capillaries that span the alveoli, while part of the carbon dioxide dissolved in the blood diffuses into the alveoli and is released into the environment with the exhalation.
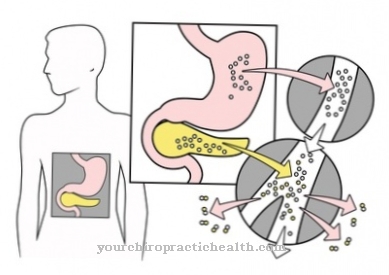
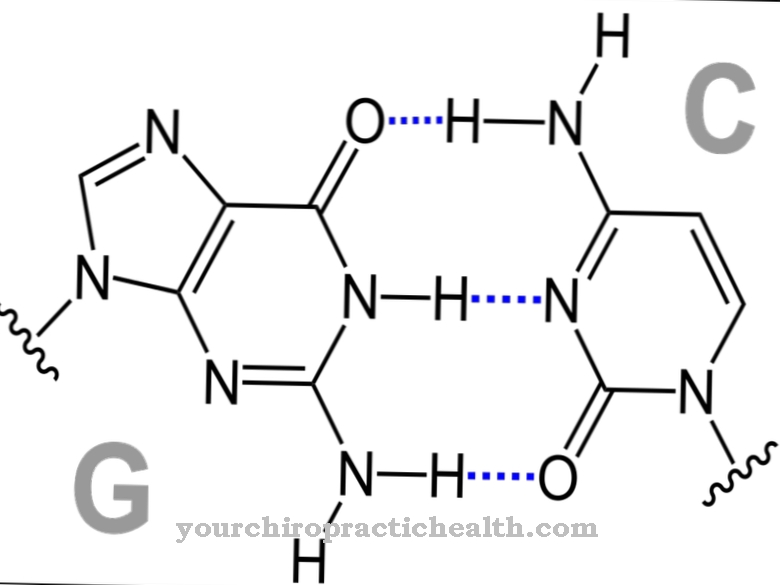
The alveoli exchange the carbon dioxide, which has already been used energetically by the cells, for oxygen. The carbon dioxide is created when the cells generate energy. In a multi-stage, catalytically controlled, enzymatic combustion process of carbohydrates (cell respiration), the main waste products are water and carbon dioxide.
The part of the airflow that goes directly into the alveoli is called alveolar ventilation. The part of the inhaled air that does not directly participate in gas exchange because it fills supporting organs such as the windpipe and bronchi is called dead space ventilation. The proportion of dead space ventilation in the total volume of air inhaled with a normal breath (tidal volume) makes up almost a third.
Function & task
The main task of ventilation is to make molecular oxygen available for cellular respiration and to remove the carbon dioxide left over from cellular respiration. The ventilation thus has a clear support function for cell respiration. This not only applies to alveolar ventilation, but also to dead space ventilation.
Anatomically, in addition to the bronchi and the windpipe (trachea), the nasal and pharynx are also part of the so-called dead space. In the context of ventilation, the dead space takes on important functions such as filtering out solid particles (dust) and sometimes also filtering out pathogenic germs in the nose.
The air intended for gas exchange is warmed up or cooled down to body temperature, depending on the ambient temperature, and the inhaled air is saturated with water vapor so that 100% relative humidity is reached. The air that flows into the alveoli is already optimally conditioned so that the best possible gas exchange can take place.
Another task of ventilation is to ventilate the entire respiratory system. If there is little physical activity or if you are bedridden, ventilation requirements are low, so that the affected people usually breathe very shallowly and when lying on the side in conjunction with shallow breathing, not all corners of the lungs and dead space are ventilated. This promotes bacterial accumulation and bacterial growth so that the ventilation can no longer fully perform its flushing function. The protective function of the ventilation is therefore only available to a limited extent.
Targeted breathing exercises can help in such cases.If you are bedridden, it makes sense to change your position from time to time in order to repeatedly ventilate other areas of the lungs.
Involuntary ventilation is mainly controlled by the respiratory center in the [[medulla oblongata [[. The medulla oblongata lies between the midbrain (mesencephalon) and the spinal cord. In addition to the breathing center, other control centers are also located there. In addition to the respiratory center, ventilation can also be controlled consciously through the breathing rate and tidal volume.
You can find your medication here
➔ Medication for shortness of breath and lung problemsIllnesses & ailments
A functioning ventilation is essential for human survival. A suspension of breathing leads to serious problems due to insufficient oxygen supply (hypoxia) after just a few minutes. Many organic diseases are known to make breathing difficult, even though the neural control center is completely intact. A common cause of breathing difficulties is bronchial asthma, which is triggered by an overreaction of the immune system to certain substances and in extreme cases can lead to spasms and attacks of suffocation.
Acute heart diseases associated with heart failure can also cause pulmonary edema with water retention in the lungs, which can lead to impaired ventilation and even shortness of breath.
With chronic bronchitis or pneumonia, there are breathing difficulties that are caused by the diseased respiratory organs themselves. If blood clots (thrombi) have formed anywhere in the body that can be carried by the bloodstream, pulmonary embolism can occur as soon as the thrombus becomes lodged in an artery that supplies the lungs and clogs them. If there is an occlusion of an artery that supplies a large part of the lungs, the embolism can quickly become life-threatening.
Changes in and abnormal ventilation can also be caused by diseases of other organs. In the case of pathological anemia (anemia), the oxygen transport is restricted, which can trigger symptoms of shortness of breath due to the high concentration of carbon dioxide. Similar symptoms can occur with severe hypoglycaemia due to type I diabetes. Typically, because of the acidification of the blood, this leads to deeper breathing without a break, which is also known as Kussmaul breathing.
Strokes or inflammation of the brain (encephalitis) or disorders of the nervous system due to drugs, neurotoxins or often also due to strong psychological pressure can cause abnormal breathing patterns up to gasping. A gasp is often a warning sign and can herald an impending respiratory arrest.