Cardiac arrhythmias occur when the heartbeat becomes irregular due to increased or decreased impulses. In the ventricular tachycardia it is a dangerous form of cardiac arrhythmia. It arises in the ventricles and is always a serious emergency.
What is ventricular tachycardia?

Ventricular tachycardia is a form of cardiac arrhythmia. It occurs when the ventricles send additional impulses that cause more than 120 heartbeats per minute. In most cases it arises from existing coronary heart disease. Depending on the speed of the heartbeat, it can lead to ventricular flutter or even to ventricular fibrillation. Therefore, a ventricular tachycardia should be treated by an emergency doctor as soon as possible, otherwise it can be fatal within a few minutes.
causes
The ventricular tachycardia is usually based on a coronary heart disease. Again, these are mostly narrowing of the coronary arteries (vessels that supply oxygen-rich blood to the heart). These constrictions in turn mean that the heart muscle can no longer be properly supplied with blood.
The constrictions themselves express themselves as a feeling of pressure and a tightness in the chest as well as heart pain, which can occur both during exercise and at rest. Coronary heart disease is favored by several factors. Smokers, people who are overweight and mostly male people of advanced age fall into the risk group. Existing diseases such as diabetes, high blood lipid levels (cholesterol) or high blood pressure as well as coronary heart disease in first-degree relatives are also considered to be major risk factors. External influences such as stress, lack of exercise and an unhealthy diet also have a harmful effect on the blood vessels.
In addition to coronary heart disease, there are other possible causes of ventricular tachycardia. Above all, there are heart muscle diseases (cardiomyopathies), which are based on a functional disorder of the heart. Cardiomyopathies are usually accompanied by an enlargement of the heart, which has a decisive influence on the heart rhythm.
Ventricular tachycardia can also arise from an inflammation of the heart muscle (myocarditis) or an existing long QT syndrome (extended QT interval in the ECG). It can also result from congenital or acquired heart defects that affect the functioning of the heart. They can also be caused by the effects of certain medications, pulmonary embolism and the derailment of certain electrolytes (e.g. potassium).
You can find your medication here
➔ Medicines to strengthen the heart and circulatory systemSymptoms, ailments & signs
Ventricular tachycardia rarely occurs in healthy people. Mostly people with previous illnesses are affected. For example, an overactive thyroid and an overdose of digitalis can promote disease. Organic heart damage also promotes a rhythm disorder. The following symptoms can escalate to cardiac arrest. Life is threatened.
Patients regularly complain of dizziness and fainting at an early stage. In addition, there are symptoms in the chest area. Sick people often describe that they feel their own heartbeat and that it has an unusual frequency. In this context, experts usually diagnose an accelerated heartbeat.
In addition, there are psychological signs. Sufferers complain of anxiety states that take on life-threatening forms. Sudden sweats and an immediate weakness of the entire body characterize the condition. In the context of ventricular tachycardia, there are also respiratory symptoms. These range from slight breathing difficulties to respiratory arrest.
Patients are getting insufficient air and gasping for it; If the condition remains untreated for a long period of time, breathing comes to a complete standstill. Problems catching air can regularly lead to cardiac arrest. Those affected should therefore immediately consult a doctor or alert an ambulance service.
Complications
The most dangerous complication of ventricular tachycardia is the threat of ventricular fibrillation. Since this achieves a heart rate that exceeds 320 beats per minute, the patient's life is in acute danger. Due to the rapidity of the heartbeat, on the one hand the heart does not have time to fill up sufficiently with blood between the beats, on the other hand the heart muscle is exhausted due to the extremely high performance.
If the oxygen-enriched blood is not pumped into the aorta in sufficient quantities, the heart will soon lack important nutrients as the blood circulation is interrupted. A vicious circle begins which brings the heart more and more out of its natural rhythm, because the contractions no longer come about in this state. With ventricular fibrillation, the heart no longer pumps, it just trembles. If this emergency is not dealt with quickly, the heart becomes completely exhausted and cardiac arrest occurs.
Another complication affects patients with long QT syndrome. If you experience cardiac arrest after ventricular fibrillation, this cannot be reversed even by attempting resuscitation. There is a final cardiac arrest after which the patient can no longer be resuscitated.
When should you go to the doctor?
If palpitations, palpitations or heart palpitations persist for several days, a doctor should be consulted for clarification. People who suffer from diabetes or high blood pressure should measure their blood pressure and pulse several times a day and note the values so that they can be presented to the treating doctor if necessary.
Under no circumstances should people who have cardiac arrhythmias persist for a long time and who experience dizziness, shortness of breath or an oppressive feeling of fear in addition to the symptoms of ventricular tachycardia.
Passers-by who see an unconscious person or relatives who are in their vicinity at the time of the emergency should immediately call an emergency doctor for help. The affected person could have ventricular tachycardia. If help arrives soon enough, it can save your life! Even if the unconsciousness only lasts for a short time, those affected are by no means out of danger.
diagnosis
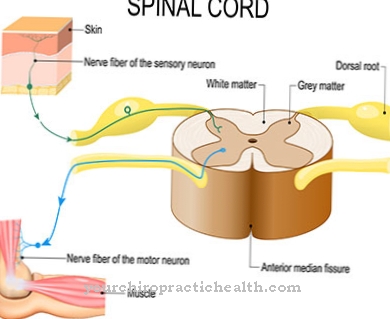
Ventricular tachycardia can be determined using an electrocardiogram (EKG). Every curve recorded by the device gives the doctor an overview of all the activities of the heart muscle fibers. The EKG records the length and duration of various phases that the heart goes through during each pump stroke.
For this purpose, several electrodes are attached to the patient's chest, which transmit the impulses to the ECG device. The latter records the pumps and displays them as wavy lines. Typical signs of ventricular tachycardia are distorted, wide ventricular complexes that last longer than 0.14 seconds. These occur independently of the atrial action. Doctors speak of an AV dissociation, as this independence shows that the ventricles and atria are no longer working synchronously with each other.
If the AV dissociation is not complete, the ECG records a normal spread of excitation in the heart chamber (QRS complex). These segments occurring in the context of a ventricular tachycardia are also referred to as “capture beat”.
Treatment & Therapy
Treatment of ventricular tachycardias depends on their cause. If it is caused by an organic disorder of the heart (e.g. myocarditis or heart failure), it must be corrected with medication or surgery. In drug therapy, a precise distinction must be made as to whether there is heart failure. In parallel to the ongoing emergency medical treatment, the patient's breathing should be secured by administering oxygen through a nasogastric tube.
If cardiac arrest occurs as a result of severe ventricular tachycardia, immediate cardioversion must be carried out using a defibrillator. The emergency doctor gives the heart electric shocks to stimulate it and make it beat again.
If the patient is unconscious, the doctor must defibrillate without the time-consuming connection of an ECG in order to save the patient's life in time.
Outlook & forecast
Typically, people who have had a previous structural heart disease will have ventricular tachycardia. Heart attack patients are an example. If ventricular tachycardia persists for more than three months after the heart attack, these patients have the worst prognosis.
Expressed in numbers, the mortality rate (lethality) within one year after the infarction is 85%. On the other hand, if ventricular tachycardias occur in people who have not had any prior heart disease, there is no increased risk of death compared to the average population.
You can find your medication here
➔ Medicines to strengthen the heart and circulatory systemprevention
Since ventricular tachycardias are life-threatening emergencies, the cause must be determined as quickly as possible so that they no longer occur in the future. Heart diseases must be treated and stressful situations avoided.
If ventricular tachycardias recur frequently in a patient despite all therapeutic measures, implantation of a defibrillator is possible. These small systems are called “implantable cardioverter defibrillators” (short: ICD). They are able to recognize a ventricular tachycardia and treat it automatically with small electrical surges.
However, in order to prevent the device from having to intervene frequently, catheter ablation should be used to try to prevent frequently recurring tachycardias. This method removes tissue that is sending false impulses to the heart, causing the heart rate to rise.
Aftercare
Follow-up treatment of the patient is of great importance if the causes of the ventricular tachycardia are diseases of the heart muscle or a coronary artery disease. As drug therapy, antiarrhythmic drugs are prescribed in order to lower the excitability of the heart. If this does not help, a catheter ablation is performed.
A catheter is inserted into the heart through the patient's groin. Pathological heart muscle cells that trigger abnormal excitations, or pathological pathways, are obliterated with the help of electric shocks. The heart then beats in its physiological rhythm again. In most cases the success of this treatment is permanent and is monitored by a long-term EKG.
If the risk of a new ventricular tachycardia, which could result in death, is too high, the patient is given an implantable cardioverter defibrillator. This is inserted under the skin of the chest and connected to the atrium and ventricle of the heart by probes. He continuously monitors the heart's activity. If the defibrillator detects a dangerous rhythm disturbance, it brings the heart back into its normal rhythm with a direct current pulse.
The patient can positively influence his follow-up treatment by preventing his heart rate from increasing unnecessarily. Coffee, nicotine and stressful situations must be avoided. Instead, moderate exercise and relaxation exercises, such as yoga, are in the foreground.
You can do that yourself
As already mentioned, ventricular tachycardias result in most cases from existing heart disease. In addition to medical treatment, these heart patients can do a lot to help prevent tachycardia. Above all, excessive stress should be reduced. Stress can be overcome particularly well through physical activity, because exercise releases so-called happiness hormones that contribute to relaxation.
Gentle activities such as a long walk in the fresh air are also suitable for beginners. In the case of emotional distress, relaxation exercises such as yoga or meditation should also be tried. If this does not achieve sufficient relaxation, there should be no hesitation in seeking psychological help. Emotional distress causes high blood pressure, among other things, which in turn can lead to tachycardia.
In addition, a healthy, balanced diet should be observed, as the heart is also heavily stressed when you are overweight. In addition to being overweight, eating high-fat foods carries the risk of increasing the cholesterol level and, with it, the fat content in the blood. This settles in the inner walls of the blood vessels and can lead to dangerous constrictions, through which the heart can no longer be optimally supplied with blood.
In addition, if you have a heart disease, you should refrain from consuming nicotine and caffeine. While caffeine has a stimulating effect and increases the heart rate, smokers with nicotine inhale pure poison that beats on both the heart and the lungs.