The Waardenburg syndrome is a congenital disease that medicine subordinates to leucism and divides it into four different types. Typical signs are numbness, malformations and pigment disorders. Since Waardenburg syndrome is a genetic disease, it cannot be treated as a cause.
What is Waardenburg Syndrome?
At the Waardenburg syndrome is a type of leucism that lay people often confuse with albinism. Both leucism and albinism are characterized by a lack of pigment. The Waardenburg syndrome owes its name to Petrus Johannes von Waardenburg, who was the first to describe the disease in 1951.
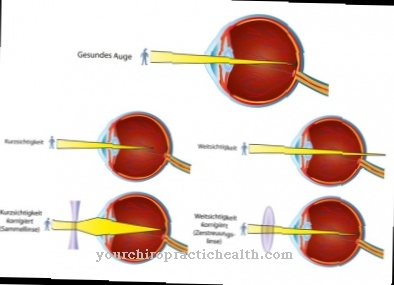
A person with leucism has no melanocytes, i.e. no skin cells that form pigments. The majority of melanocytes are in the epidermis and around the hair follicles. The pigments are not only found in the skin, but also in the eyes, where the retina and iris also form pigments. They are not only used for visual design.
They protect the skin or the cells of the eye from excessive exposure to light. The color melanin can be either brown to black or yellow to reddish. As a rule, there are mixtures of both variants, which form the characteristic color image of the pigment cells.
causes
Waardenburg syndrome is due to a mutation in the genetic make-up. Deoxyribonucleic acid (DNA) shows deviations compared to healthy DNA. Depending on the gene affected, the disease manifests itself in different ways. Type I and type III (Klein-Waardenburg syndrome) are due to a mutation in the PAX gene at the 2Q35 gene location.
In type II, the MITF gene is responsible for inheriting the syndrome. Different gene segments can be mutated there. Sometimes medicine therefore further differentiates type III into subtypes A, B, C and D. Externally, however, the subtypes hardly appear to differ from one another. For type IV, different gene segments on the endothelin-3 gene or the endothelin-B receptor gene are also possible as mutation sites.
All four types of Waardenburg syndrome are autosomal, which means they are on one of the autosomes, not on the X or Y chromosome. Types I, II and III are recessive: the syndrome only manifests itself when the double set of chromosomes has two disease-carrying genes. However, if a person not only has a mutated but also a healthy gene segment, the disease does not break out. Such a person can still pass Waardenburg syndrome on to their children.
Symptoms, ailments & signs
The most noticeable symptom of Waardenburg syndrome is the pigment disorder, which is mainly reflected in three areas. The forelock is colorless in people with Waardenburg syndrome and therefore appears white. The eyes have different colors, because the irises of both eyes do not form pigments in every place.
Areas that do not contain pigment appear blue in the iris. The remaining areas form the dyes as they are genetically determined. Medicine also calls this phenomenon iris heterochromia. In addition to the white forelock and iris heterochromia, Waardenburg syndrome type I also manifests itself as white spot disease or check skin (vitiligo).
Doctors use it to describe the pigment deficiency in the skin, which is particularly evident on the hands, neck, face and anogenital area. In addition, deafness and malformations manifest themselves in the face: a high and wide root of the nose are just as characteristic as tissues or organs that form in the wrong place (dystopia canthorum).
Dystopia canthorum does not occur in type II of Waardenburg syndrome, although type II otherwise corresponds to type I. Type III has all symptoms of type I; in addition, malformations of the arms occur. The most serious form of Waardenburg syndrome is found in type IV, which often leads to the death of the person affected.
The differentiation of certain neurons is also disturbed in this form of the disease, which also leads to the development of Hirschsprung's disease (congenital megacolon). This intestinal disease manifests itself, among other things, in the narrowing of the large intestine.
Diagnosis & course of disease
Waardenburg syndrome is congenital. The mutation disrupts proper development early on in the development of the child in the womb, from which the various symptoms arise. Doctors cannot diagnose Waardenburg syndrome just based on its external characteristics: they can use a genetic test to clarify whether one of the mutations that trigger the syndrome is present.
Complications
Waardenburg syndrome can lead to various complications. A typical consequence of the disease is the characteristic pigment disorder. Depending on how severe it is and at what age it first appears, this noticeable blemish can result in serious psychological problems. Those affected often develop social anxiety or even full-blown depression.
In the case of Waardenburg syndrome type I, white spot disease also occurs, which can exacerbate the mental suffering mentioned. Furthermore, in the course of the disease, hearing loss and malformations of the face can occur. A possible secondary disease of Waardenburg syndrome is Hirschsprung's disease. This bowel disease is associated with narrowing of the colon.
Serious gastrointestinal complaints can occur, which can manifest themselves in constipation or even in an intestinal obstruction. Since the syndrome is hereditary, there are hardly any treatment options and the disease often takes a severe course, which is associated with permanent cognitive and aesthetic impairments for those affected.
Symptomatic therapy is also not free of risk. The administration of cortisone can cause skin irritation and other side effects. Surgical interventions, such as those used in the treatment of intestinal complaints, are always associated with a risk of infection and injury.
When should you go to the doctor?
Since Waardenburg syndrome cannot cure independently, the person affected should consult a doctor. Early detection and subsequent treatment of the disease always has a very positive effect on the further course and can also prevent further complications. A medical professional should therefore be contacted at the first signs and symptoms of the syndrome. A doctor should be consulted if the person concerned suffers from a severe pigment disorder. This often results in completely colorless skin, which appears very white.
White spots can also develop on the skin. Most patients also suffer from a hearing loss due to Waardenburg syndrome, which does not go away on its own. Likewise, the organs in the body are incorrectly arranged, which can lead to severe complications. Waardenburg syndrome can be recognized by a pediatrician or a general practitioner. Further treatment depends very much on the type and severity of the symptoms, so that no general prediction can be made about the further course of the disease. Since the syndrome can often lead to mental upsets, a visit to a psychologist is also very useful.
Treatment & Therapy
Since Waardenburg syndrome is a hereditary disease, a causal treatment is not possible. Measures that alleviate the hearing loss may be possible. The exact procedure, however, depends on the individual situation. In the more severe type IV, doctors must also treat Hirschsprung's disease.
prevention
Targeted prevention is not possible with Waardenburg syndrome, as it is a hereditary disease. Type IV of Waardenburg syndrome follows an autosomal recessive inheritance. The disease therefore only manifests itself when the child inherits an allele carrying the disease from both parents. However, if the genome contains only one diseased and one healthy allele, Waardenburg syndrome does not break out.
Types I – III inheritance, on the other hand, is autosomal dominant: if a person has a mutated and a healthy gene, the disease manifests itself. However, this person does not necessarily have to pass Waardenburg syndrome on to their child, as they can also pass on the healthy gene. Chance determines whether a parent passes the disease-carrying gene or the healthy gene on to their child.
Aftercare
Waardenburg syndrome requires extensive follow-up care. Since it is a congenital disease, a causal treatment is not possible. Follow-up care focuses on advising the patient on further therapeutic measures. The pigment disorders and the inner ear hearing loss must be checked by a doctor at regular intervals.
Follow-up care consists of a patient interview and a physical examination. When taking the anamnesis, the doctor first gets an idea of the current symptoms. Complaints that have largely subsided do not require any further follow-up care. Pigment disorders and hearing impairment are chronic conditions that must be monitored regularly.
If necessary, new therapeutic measures arise between the check-ups that are suitable for the patient. The patient should keep a complaint diary and note any unusual symptoms in it. With the help of the notes, regular follow-up care can be optimally aligned with the symptoms. Depending on the nature of the complaints, therapeutic help may also have to be sought. Since the syndrome can develop very differently, the measures must be determined individually.
You can do that yourself
The medical treatment of Waardenburg syndrome can be supported by various self-help measures. The typical inner ear hearing loss can be compensated by wearing a hearing aid. Relatives must speak loudly and clearly and face the patient as they speak so that they can lip read.
In order to avoid misunderstandings, it is advisable to deal openly with the hearing impairment. This also applies to other symptoms of the disease, such as pigmentation disorders and visual disorders, which can develop in the course of life. Sick people should inform themselves in detail about the ptosis-epicanthus syndrome and decide together with the doctor which remedies will help against the individual symptoms.
Most of the time, very different complaints occur, which can sometimes also represent emotional stress. Therapeutic support is just as important for the patient as physical treatment, especially in the case of depressive moods or anxiety disorders. Parents of children with Waardenburg syndrome should arrange for a genetic test. Often the cause of the hereditary disease can be determined, which makes planning more children easier. If the complaints have a strong negative effect on well-being, it can also be useful to visit a self-help group. The Leona e.V. association provides those affected with further contact points.


.jpg)
.jpg)

.jpg)







.jpg)




.jpg)


