The Spondylolisthesis is a spinal disease in which one or more vertebral bodies shift against each other (Vortex sliding) and thus lead to a loss of stability of the spine. Depending on the extent and progression of the disease (involvement of the nerves, spinal canal stenosis), spondylolisthesis can usually be treated well within the framework of conservative measures.
What is vortex sliding?
.jpg)
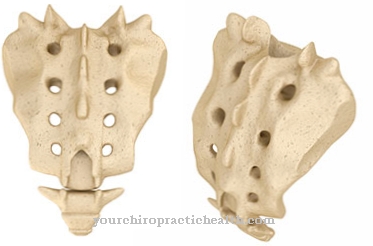
As Vortex sliding or. Spondylolisthesis is the term used to describe the gliding of a corpus vertebrae (vertebral body) over the vertebral body below, which can be differentiated according to acquired (wear and tear, trauma, overload) and genetically determined forms (spondylolysis).
The vertebrae can be shifted either forwards (ventrolisthesis or anterolisthesis) or backwards (retrolisthesis). In most cases, the lumbar vertebrae, especially the 5th lumbar vertebra, are affected by spondylolisthesis, which is often asymptomatic and does not cause any symptoms.
Spondylolisthesis can manifest itself in the form of stress-dependent back and lower back pain as well as a feeling of instability in the affected area. In rare cases, a narrowing of the spinal canal may result in root compression syndrome (irritation of the root of a spinal nerve in the affected area of the spine), which leads to neurological symptoms.
causes
A Spondylolisthesis can either be genetic or acquired. Age-related changes in the spine, especially the intervertebral discs, which lose height with age, cause the ligaments that stabilize the spine to lose their elasticity.
As a result, the vertebral bodies lose their stability, so that they can shift against each other (degenerative vertebral sliding). This process of wear and tear is favored by insufficient movement and weak core muscles. In addition, fatigue lesions or fractures in the pars interarticularis of the vertebral arch as a result of excessive stress on the spine (usually in competitive sports such as javelin throwing, pole vaulting, weight lifting) can lead to vertebral sliding (isthmic spondylolisthesis).
In addition, severe trauma with injuries to the spine or surgery on the spine can cause vertebral slippage (post-traumatic spondylolisthesis). If the structure of the spine is disturbed as a result of congenital defects in the vertebral arches (spondylolysis), this is referred to as congenital or dysplastic vertebral sliding. In rare cases, the sliding of the vertebrae can be attributed to a tumor or an inflammation (pathological spondylolisthesis).
Symptoms, ailments & signs
Sliding vertebrae can lead to various symptoms and complaints. However, it is possible that non-specific low back pain occurs only occasionally. These were mostly caused by the load. It even happens that a spondylolisthesis is completely symptom-free. In this case, it is often diagnosed only by chance. Whether the freedom from complaints will be maintained over the years is another question.
The resulting symptoms of spondylolisthesis are caused by the sliding of the vertebrae. There is a feeling of pressure and pain in the lumbar spine area. These can also radiate into the thigh. In other cases, there is sciatica pain. These are often attributed to other events and not necessarily to the spondylolisthesis.
Occasionally, during the course of the spondylolisthesis, feelings of tension or muscle cramps occur in the legs. There, the gliding vertebrae can also make themselves felt through muscle weakness. Even this symptom does not necessarily indicate sliding vertebrae. Since there are four degrees of severity of sliding vertebrae, the symptoms can be mild, moderate or severe. The instability symptoms can suddenly worsen under stress.
Some symptoms suggest that nerves are involved in the pain. Much more often, however, the slipping of the vertebrae is the cause of further symptoms, for example after a herniated disc or a facet joint arthrosis. Both are characterized by severe pain deep in the lower back.
Diagnosis & course
A Spondylolisthesis is usually diagnosed using an X-ray. Here, vertebral sliding in the side view can be seen in the form of a movement-independent fixed displacement of the affected vertebral body.
At the same time, statements can be made about the severity of the spondylolisthesis (graduation according to Meyerding) and changes in the spine (curvatures, arthrosis, changes in the intervertebral discs, osteoporosis). Computer and magnetic resonance imaging are also used to determine whether soft tissues or nerves are involved.
In some cases, congenital vertebral slippage in the advanced stage can be diagnosed using the gait pattern (tightrope walk). A spondylolisthesis has a good prognosis depending on the presence of other impairments (involvement of the nerves, spinal canal stenosis) and can be treated well in the context of conservative measures in the case of minor complaints.
Complications
Anyone who has gliding vertebrae also knows them under terms such as gliding vertebrae or spondylolisthesis. Acquired disease of the spine most often affects the fourth or fifth lumbar vertebrae. Since vertebral sliding is divided into four degrees of severity - from Meyerding I to IV - complications are not uncommon with higher degrees of severity.
One of the most common complications of sliding vertebrae is severe lower back pain, which defies any physiotherapeutic treatment. In the event of such complications, surgical interventions are a solution. In the case of severe spondylolisthesis or spondyloptosis with pain lasting more than six months, surgery may be necessary.
Surgical stiffening of the gliding vertebrae is an option. The direct screwing of the spondylolysis in the vertebral arch can already be carried out in severely affected children. Scars and nerve injuries can occur as a result of this operation. Often times, when the stiffened vertebral joints are loaded again, screws break. These will require further surgery.
The acquired instability of the spine can pinch nerves in the spinal canal. In addition, surrounding nerves can be overstretched. Nerve damage or functional failures in the area of the surrounding nerves can occur. As a result of the pressure on nerve cords, paralysis is possible. These can affect the legs, but also the bladder and other digestive organs. The sliding vertebrae also wear and tear on the affected intervertebral discs and vertebral joints.
When should you go to the doctor?
If the person concerned complains of pain or irregularities in the back, this should be observed further. In the case of a one-off situation of overload or an incorrect load on the skeletal system, improvements can be seen within a short period of time after sufficient rest and rest. If after a night's sleep it is found that the patient is free of symptoms, in most cases the person concerned does not need a medical consultation.
However, if the discrepancies in the back area show a steady increase or if they continue unabated over a longer period of time, a doctor should be consulted. Restrictions in mobility and disorders in general movement sequences indicate a health disorder. Muscle complaints, feelings of tension and a continuous decline in physical performance should be examined and treated. Although there are phases of freedom from symptoms in some of those affected, action is required as soon as the impairment develops sporadically.
If you feel tension or feel uncomfortable when you apply slight pressure to your back, you need to see a doctor. These are warning signals from the organism that require medical care. If the person concerned has the overall feeling of instability in the area of the spine, it is advisable to visit a doctor for a check-up. The perceptions should be discussed so that medical tests can be initiated.
Treatment & Therapy
A Spondylolisthesis is initially treated conservatively in most cases. Conservative therapy aims to reduce the pain present through pain-relieving medication and to strengthen the core muscles through physiotherapeutic, physical and physiotherapy measures.
To relieve and stabilize the spine, the core and abdominal muscles are trained individually as part of physiotherapy. For regular exercise, which is a basic component of therapy, back-friendly sports such as cycling, back swimming and Nordic walking are also recommended. In some cases, a corset (Lindemann bodice) is also used to stabilize the spine and reduce pain immediately, although this should only be worn for a short time to avoid weakening the core muscles.
Physical measures such as massages also help to reduce pain, while back training can contribute to a spine and intervertebral disc-friendly gait and everyday behavior. If, despite conservative therapy, there is no improvement in symptoms after 6 months, or if there is involvement of the nerves or spinal stenosis, surgical intervention may be indicated.
In spinal canal stenosis, for example, the spinal canal can be widened as part of a laminectomy or surgical decompression and the unstable vertebral bodies stiffened (spondylodesis). In adolescents with pronounced congenital sliding of the vertebrae, the affected vertebra is returned to its original position (reduction) in advance of the spondylodesis.
You can find your medication here
➔ Medicines for back painprevention
One Spondylolisthesis can only be prevented to a limited extent. However, strengthened and trained core muscles, everyday behavior that is gentle on the spine and intervertebral discs, and regular exercise help minimize the risk of vertebral slipping and slow the progression of spondylolisthesis.
Aftercare
Follow-up care plays an important role in both conservative and surgical treatment of sliding vertebrae. Conservative therapy is followed by orthopedic rehabilitation measures, which either the family doctor or an orthopedist accompanies. The conservative measures are usually considered more promising than surgical interventions.
For the follow-up treatment of a spondylolisthesis, physiotherapy exercises have proven themselves as rehabilitation measures, which can be combined with sporting activities, relaxation exercises and psychotherapy. The rehab includes an intensive program that takes several weeks to complete. To do this, however, the patient must no longer suffer from acute pain.
For this purpose, he receives pain medication and muscle relaxing preparations. The freedom from pain means that the patient can move regularly again and train his muscles. The focus is on building up the back and abdominal muscles. The cooperation of the patient is also extremely important for the success of the treatment. If the vertebral slippage has to be treated surgically, follow-up treatment is also required. Depending on the extent of the procedure, the patient stays in the clinic for about a week.
It usually takes twelve weeks for rehabilitation to begin so that the body has ample opportunity to recover. After gradually taking off the stabilizing corset, physiotherapy exercises begin to strengthen the back muscles. A check-up also takes place three months after the operation, during which the spinal stability is checked.
You can do that yourself
People with vertebral slippage (spondylolisthesis) have the opportunity in everyday life to take various measures to reduce their symptoms and to prevent their disease from worsening. In numerous cases, certain sports are the trigger for vertebral sliding, so that those affected first start at this point.
It is advisable to reduce the intensity of exercise and to contact a physiotherapist. Doing certain exercises before actually exercising can help reduce the risk of deterioration. In general, it is helpful to seek physiotherapy treatment and specifically strengthen the muscles near the affected section of the spine with professional support. This also reduces symptoms and improves the prognosis. The patient, his trainer and the physiotherapist must jointly decide whether a change in sport is necessary in individual cases.
Exercising less back-stressing sporting activities makes sense in any case and usually has a beneficial effect on the state of health. Patients are sometimes asked to wear a corset for a while to support the spine.Those affected should comply with this recommendation in their own interest, even if this is associated with temporary restrictions in everyday life and when exercising.

.jpg)
.jpg)









.jpg)




.jpg)


