At Herpes zoster oticus it is a second disease with the varicella-zoster virus. The symptoms show up in the ear region.
What is zoster oticus?
Herpes zoster oticus is a special form of shingles (herpes zoster). What is meant is an infectious disease in the course of which inactive herpes viruses become active again in the ganglia of the central nervous system (CNS). About 90 percent of the population suffers from the varicella zoster virus.
The initial infection occurs in the form of chickenpox (varicella). There is then an immunity to chickenpox that lasts for the rest of life. However, around 20 percent of all patients can develop shingles later on. People over 40 years of age are particularly affected. In some cases, shingles is accompanied by otic zoster. There are no differences between men and women.
causes
Zoster oticus is triggered by the varicella zoster virus. This is also called the human herpes 3 virus. It belongs to the group of herpes viruses. The globally occurring pathogen is equipped with a double-stranded DNA including a lipid shell. The varicella zoster virus primarily affects nerve cells.
The germ is able to survive in the nerve nodes of the spinal canal for a period of several years. The transmission to humans takes place through droplet infection. After the initial infection with chickenpox, the causative viruses migrate along the nerve fibers into the spinal ganglia. There they can survive and are only reactivated after years or even decades.
Because larger areas of the spinal ganglia are destroyed during reactivation, this results in acute pain, also known as zoster pain. Possible reasons for reactivating the virus are disorders of the immune system, a reduction in the strength of the immune system for reasons of age or immunosuppression, in which the immune system is deliberately reduced as part of a transplant.
Immune system diseases such as AIDS (HIV) can also result in a defective immune system. Other conceivable triggers are toxic substances, severe infections such as rabies, UV rays or X-rays. In addition, a transmission with the varicella zoster virus is on People who have not yet had chickenpox are possible.
Symptoms, ailments & signs
Herpes zoster oticus is noticeable in the early stages through tiredness as well as headache and body aches. A typical symptom of the disease is the appearance of vesicles on the earlobes. They also show up in the outer ear canal and sometimes in the inner eardrum.
Sometimes they also appear on the tongue, soft palate, and sides of the neck. The bubbles reach the size of the head of a pin or a grain of rice. The water-clear, tense and plump vesicles resemble pearls. They show up as a sharp reddening of the skin and appear within two to three days.
After a period of two to seven days, the contents of the vesicles take on a yellowish, purulent color, while the reddening slowly subsides. After the vesicles have dried out after about a week, a yellowish or brownish crust appears. The disease lasts about two to three weeks and then goes back. It is not uncommon for scars to appear in the form of light or dark patches of skin.
The so-called zoster pain appears during the illness within the ear, in the neck or in the side of the face. About two thirds of all patients also suffer from facial palsy on one side of the face. The corners of the mouth hang down, the eyelid cannot be completely closed and the forehead cannot be wrinkled.
Diagnosis & course of disease
In order to diagnose herpes zoster, the doctor pays attention to the patient's symptoms. Typical signs are the redness and the formation of blisters on the ear. Further investigations are only required in problem cases. It is also possible to detect the causative agent.
This process takes place via the polymerase chain reaction from the contents of the vesicles or from affected tissue. Furthermore, it is possible to detect specific antibodies of the pathogen, but this is not considered to be particularly meaningful because the viruses are already present in the body.
In most cases, herpes zoster oticus takes a positive course. Healing proceeds without any problems in two thirds of all patients. Relapses are rare. In people over 60 years of age, however, the disease can last for a long time. The course of the disease is considered unfavorable if people with immunodeficiency are affected by zoster oticus.
Complications
Herpes zoster oticus can cause various complications. The typical secondary symptoms include headache and body aches. Most people also have vesicles on the earlobes that can become infected. If the vesicles spread into the inner eardrum, hearing problems and temporary deafness can occur. If the vesicles appear on the tongue or roof of the mouth, it will cause problems with eating.
Malnutrition with its typical complications and consequences can result from this. If the blisters are scratched open, this can lead to the formation of scars. The so-called zoster pain accompanies these symptoms.
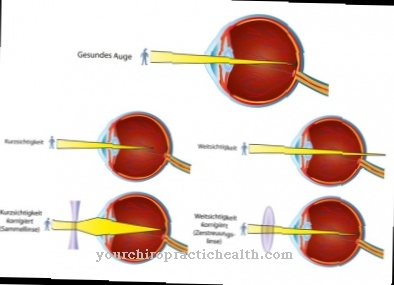
This characteristic pain in the face and neck area increases as the disease progresses and is associated with visual field defects such as drooping corners of the mouth. Major complications are unlikely to occur when treating herpes zoster. Problems can arise if the person concerned has an allergic reaction to proven drugs such as valaciclovir or brivudine.
In addition, side effects and interactions can occur, for example, in individual cases, depressive moods or physical complaints such as headaches, body aches and gastrointestinal problems occur. Serious complications require hospital treatment.
When should you go to the doctor?
If the person concerned is suffering from inexplicable tiredness, a general feeling of illness or fatigue, there is cause for concern. If these irregularities continue unabated for several days or if they increase in intensity, a doctor should be consulted. In the case of aching limbs, a decrease in physical performance or diffuse exhaustion, it is advisable to consult a doctor. Changes in the appearance of the skin and especially the formation of blisters on the face are signs of an illness.
Since zoster oticus is a viral disease, the pathogens can multiply in the organism unhindered in an untreated state and trigger an increase in symptoms. If vesicles form in the area of the ear or in the mouth, it is advisable to consult a doctor.
The sooner medical care can be initiated, the better the healing process and the more complications can be avoided. If there are complaints in the face or neck area, action is required. If you experience pain or visual disturbances, you should consult a doctor immediately. Internal weakness, emotional changes due to the visual flaw, and reddening of the skin should be examined and treated. In many cases, the complexion of the skin changes rapidly within a few hours.
Treatment & Therapy
The treatment of zoster oticus is antiviral. It is important to start the treatment no later than 72 hours after the onset of skin symptoms. Aciclovir, which can be administered in the form of tablets or as an infusion, is usually administered. Other proven agents are valaciclovir, famciclovir and brivudine, which are also antivirals.
These active ingredients combat the growth and reproduction of herpes viruses by counteracting the structure of the virus DNA. After only hours, skin symptoms and pain are successfully suppressed. To treat the pain, the patient is given pain relievers, anticonvulsants such as gabapentin, or antidepressants. Tricyclic antidepressants are particularly useful in the case of herpes zoster neuralgia. Hospital treatment is required for severe complications.
You can find your medication here
➔ Medicines for rash & eczemaprevention
A vaccination against chickenpox is considered the most sensible preventive measure against zoster oticus. If the chickenpox does not break out, herpes zoster oticus cannot occur later. The chickenpox vaccination is one of the standard vaccination procedures for children and adolescents.
Aftercare
Follow-up care for zoster oticus includes what has already been said about self-help: A healthy lifestyle helps patients to support the immune system so that it can counter a new outbreak of the infection. This is important because the varicella-zoster viruses have established themselves in the body and are still latent in the body even after an outbreak has been successfully fought.
If the immune system now becomes weaker - be it due to other serious illnesses such as cancer, due to increasing age, therapies that suppress the immune system or infections such as flu infections or gastrointestinal diseases, then the zoster viruses have it easy again Break out. Therefore, patients are advised to limit their alcohol consumption and to completely avoid nicotine.
A balanced, fresh diet is indispensable for the immune system, as is physical exercise in the fresh air, in which the heart and circulation are trained. In the case of nutrient deficiencies, the administration of appropriate food supplements helps. Patients should consult their family doctor here. In Germany, vaccines against shingles have been available for some time. These also protect against an outbreak of herpes zoster, since both shingles and zoster oticus are triggered by the same herpes viruses. Most health insurances will reimburse this vaccination, especially if the patient is over fifty years old.
You can do that yourself
In most cases of otic herpes zoster, major complications only arise when the immune system is very weak. It is therefore particularly important for the affected patients to ensure a stable immune system. This is especially true for people over the age of sixty.
The immune system is positively stimulated by giving up stimulant drugs such as alcohol and nicotine, but instead eating a balanced diet, ensuring extended rest periods and exercising in the fresh air as much as possible. It is also advisable to drink one and a half to two liters of still water daily, as it supports the excretory organs in their work and helps to expel harmful substances.
During the acute phase of herpes zoster oticus, the painful sores of the herpes zoster oticus can make it difficult for the patient to eat. But especially in immunocompromised patients, this can quickly lead to malnutrition. It is particularly important for them to eat a fresh, balanced diet. If these patients are unable to eat three to five times a day, they should inform their doctor about it. He may try to compensate for any deficiencies with dietary supplements or artificial nutrition.
During the illness phase, the patient can become depressed. In this case, the doctor will prescribe an antidepressant. Psychotherapeutic crisis intervention is also conceivable.














.jpg)




.jpg)


