Villi movements take place within the small intestine. There are finger-shaped elevations of the mucous membrane. These are called villi.
What are villi movements?

The mucous membrane of the small intestine (intestinal mucosa) lines the duodenum, jejunum and ileum. The intestinal mucosa does not form a smooth surface, but lies in folds. These folds, up to one centimeter high, are also called Kerckring folds or Plicae circulares. They are formed from the mucosa and submucosa. The muscular layer of the mucous membrane is not involved.
Another typical feature of the mucous membrane of the small intestine are the villi (villi intestinales). These are finger-shaped or leaf-shaped protuberances on the mucous membrane that are 0.5 to 1.5 millimeters high. At these points the mucous membrane shows itself with a single-layer, prismatic epithelium.
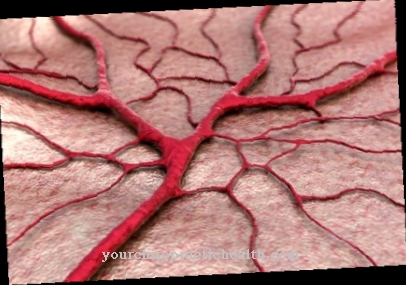
In the center of each villus there is a so-called chyle vessel and a network of many small blood vessels (capillaries). Lymph fluid flows through the chyle. In addition, muscle fibers pull into each villi. This allows the villi to move and deform. The Lieberkühn crypts are located between the villi, which secrete numerous enzymes. The cell pole of the cells that sit on the villi carries microvilli. These small cells are also known as brush cells.
Function & task
Kerckring folds, intestinal villi and microvilli serve to enlarge the surface of the small intestine. With a total length of around three to six meters, the special surface of the small intestine achieves an astonishingly large absorption area of 100 to 240 m².
That the villi are able to move independently could only be concluded from the histology of the protuberances. Each villus has smooth muscle fibers. These fibers run lengthways through the villi. From these observations, pathologists in the 19th century concluded that the villi could move. Direct observation of the villi movement was not possible until 1914. It was found that the villi contract individually and do not follow a community pattern. Around six contractions per minute per villus were observed in a dog in 1927.
It is interesting to note that the villi shorten but not get thicker. Instead, the mucous membrane wrinkles itself. This change in shape suggests that the contents of the villi are squeezed out during these contractions.
The villi serve to absorb nutrients such as sugar, protein or fat components. The contents of the villi are probably pressed into the lymphatic spaces of the submucosa.
Depending on the section of the intestine, there are 2000 to 4000 villi per square meter in humans. This number can be used to calculate which large quantities of nutrients can be absorbed thanks to the pumping villi movements.
The movements of the villi are controlled by the parasympathetic and also the sympathetic nervous system. Weak stimuli from the vagus nerve stimulate the villi to move; if the vagus nerve is strongly stimulated, the villi slacken and stop moving. The villi are also stimulated by hormones. Villikinin is a hormone that controls villi movement.
Illnesses & ailments
In many diseases of the intestine, the villi are affected. Celiac disease is a disease that damages and destroys many villi. It is a gluten intolerance. Those affected are hypersensitive to gluten, a type of adhesive protein found in many types of grain. Food containing gluten causes severe inflammation of the intestinal lining in patients. Intestinal epithelial cells and with them the villi are destroyed over a large area. Villi movement is therefore no longer possible. Nutrients can only be absorbed very poorly; most of the food remains undigested in the intestine. There is weight loss, vomiting, diarrhea or loss of appetite. Fatigue and depression can also be symptoms of celiac disease.
A similar pathophysiology and thus also similar symptoms are found in a wheat allergy. It is estimated that around one to two percent of the population is affected by the disease in industrialized nations. There is no causal treatment. The only thing left for those affected is a lifelong gluten-free diet. This allows the intestinal mucosa to recover. The villi also build up again and can move normally. This is important because otherwise there would be permanent deficiency symptoms.
Damage to the villi and limited villus mobility are also evident in the case of a deficiency in folic acid and vitamin B12. A deficiency in vitamin B12 can have various causes. Chronic gastritis (inflammation of the lining of the stomach), for example, can lead to a lack of intrinsic factor. Without the intrinsic factor, vitamin B12 cannot be absorbed in the intestine. Insufficient intake or a bad colonization of the intestine can also trigger a B12 deficiency. Inadequate DNA synthesis leads to anemia if there is a lack of folic acid and B12. Food intolerance is also common. These could be a result of the lack of villi movement.
Two diseases that are associated with villi atrophy and immobility of the intestinal villi are Microvillous inclusion disease and tufting enteropathy. Microvillary inclusion disease (MVID) is congenital. Immediately after birth, life-threatening diarrhea occurs due to the intestinal's inadequate absorption capacity. There is a risk of dehydration. The affected children often have to undergo a small bowel transplant shortly after birth. Tufting enteropathy is also congenital. It also manifests itself in severe diarrhea, and a small intestine transplant can hardly be avoided here either.























.jpg)

.jpg)
