Constraints or Obsessive-compulsive disorder are mental illnesses. The sick person suffers from obsessive thoughts and psychological stress, so that he unconsciously has to perform compulsive actions (e.g. constant hand washing). One also speaks of a mental disorder. Determining its cause is not so easy, because it can be in the psychological as well as in the organic area. In addition to psychotherapy, obsessive-compulsive disorder can also be treated with medication.
What are compulsions and obsessive-compulsive disorder?
In the Obsessive-compulsive disorder is divided into obsessions and compulsions. Obsessive-compulsive thoughts differ from normal thoughts in the way they are experienced and thought by the person concerned. The thoughts during OCD are accompanied by a constant fear of harming other people or of getting into an embarrassing situation yourself.
They cannot be turned off consciously or thought through to the end, so that, similar to a cycle, they reappear again and again and finally end in despair. The obsessions are further divided into obsessions, compulsive impulses and compulsion to brood. When imagining and brooding, the person concerned experiences a negative situation over and over again, e.g. B. that something might happen to the spouse, or that he might have misunderstood something.
The compulsive impulses drive him to carry out certain actions, even if they can have negative effects on the person concerned or on others. Obsessive-compulsive disorder is perceived as nonsensical, but any attempt to defend yourself against it triggers even more fear and tension.
In the case of obsessive-compulsive disorder, the person affected cannot defend himself against the compulsive acts. These actions are behaviors that have to be repeated so often that they interfere with everyday life. An example of behavior during an OCD is constantly checking that the stove has been turned off. In this case, the person concerned is forced to check this again and again and thus does not get to do other things.
causes
A Obsessive-compulsive disorder can appear in different forms and in different contexts. Several factors play a role in Obsessive Compulsive Disorder. On the one hand, obsessive-compulsive disorder can be caused by an organic malfunction and on the other hand by mental disorders.
Obsessive-compulsive disorder is often associated with other medical conditions. For example, in connection with multiple sclerosis or epilepsy, but also together with depressive disorders, schizophrenia and alcohol abuse, obsessive-compulsive disorder can occur. One speaks of obsessive-compulsive disorder only if it is particularly pronounced and there is no other mental illness.
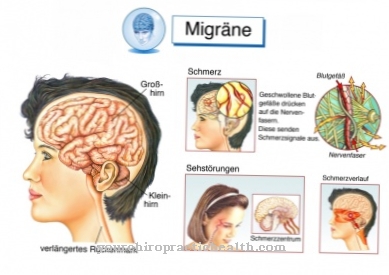
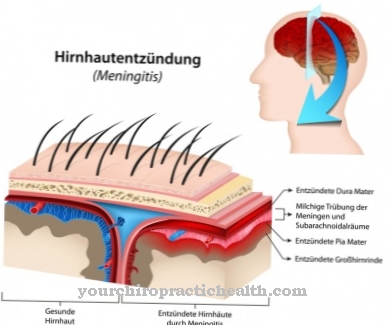
From a medical perspective, obsessive-compulsive disorder is caused by certain regions in the brain being damaged. This can be the basal ganglia, the limbic system or the frontal lobe. If the family already has OCD, this biological factor can often not be ruled out as a cause.
Typical constraints
- constant hand washing (Compulsory cleanliness) after touching objects or people
- Control constraintse.g. whether the stove is off or whether the door has really been locked
- Compulsory counting - The person concerned has to constantly count something in his environment. For example the slabs on the sidewalk or steps on a staircase
- Order - Everything must be in its place in the apartment, nothing may be dirty or otherwise arranged
- Compulsion to touch - Patients have to constantly touch a certain object or, on the contrary, that patients cannot touch a certain object at all
- verbal and acoustic constraints - For example, patients must always sing or whistle the same melody or repeat certain expressions
Symptoms, ailments & signs
Obsessive-compulsive disorder manifests itself in different ways as there are different forms of the condition. A classic, for example, is compulsory washing, in which those affected have to wash their hands again and again because contamination with dangerous bacteria is suspected even when a door handle is used harmlessly.
The need to control is also very common. Here, for example, those affected keep checking whether a stove is really switched off, even if they have already done so several times before. Counting can become just as compulsive as the habit of treading the same path over and over or performing rituals. Obsessive-compulsive thoughts, which have to be played through in the mind again and again, are also a broad field.
What all compulsions have in common is that the person affected often recognizes the absurdity of actions and thoughts, but cannot do anything about it. When resisting a coercion, the thought is often associated that something bad could happen if the coercion is not carried out correctly.
Often the compulsions of those affected are accompanied by symptoms of anxiety and a depressive mood, because the compulsion triggers shame and helplessness and often drives the patient into social isolation. With obsessive-compulsive disorder, a lot of time a day is devoted to compulsive actions and thoughts.
Diagnosis & course
The Obsessive-compulsive disorder can be diagnosed if the sick person lives with the obsessive thoughts or compulsive actions for at least two weeks and describes this condition as an unfortunate experience and experiences a reduced quality of life as a result of this situation, i.e. the obsessive-compulsive disorder significantly affects his everyday life.
Another aspect of obsessive-compulsive disorder is that the sufferer recognizes obsessive-compulsive thoughts as their own and cannot resist them. The perception of the execution of the thought or the ideas or impulses are coupled with unpleasant feelings. Obsessive-compulsive disorder can also cause physical harm, such as: E.g. when washing hands frequently, eczema develops. If the obsessive-compulsive disorder is severe, thoughts of suicide are also possible.
Complications
Compulsive obsessive-compulsive disorder can be very diverse. The extent of possible complications depends, among other things, on whether the obsessive-compulsive disorder also affects other people or even has elements of self-harm. Therapy lowers the risk of complications.
Obsessive-compulsive disorder is often a reason for social isolation, as those affected can become unable to work or are socially very limited. In combination with the high correlation between depressive moods, depression and other personality disorders associated with OCD, the risk of suicidal thoughts and the corresponding action increases.
Furthermore, the compulsory washing leads to skin damage (mostly to eczema), which can lead to other health problems. Obsessive-compulsive disorder always entails the risk that the person concerned neglects other areas of life in favor of his or her disorder (especially when it comes to the urge to constantly control certain things) and thus get into negative situations. This is also the case when it comes to obsessive-compulsive thoughts that mainly affect the immediate environment.
It is precisely those thoughts that consist of violent fantasies or inappropriate sexual fantasies that place a tremendous burden on the relationship between the person concerned and his environment.While there is no significant risk that these thoughts are implemented purely due to the OCD, numerous other personality disorders can lead to a loss of impulse control.
When should you go to the doctor?
Not every everyday ritual belongs to an obsessive-compulsive disorder that requires medical or psychotherapeutic treatment. However, sufferers should see a doctor or therapist if their everyday life suffers from unpleasant compulsions or obsessions and the compulsions last for at least two weeks. Everyday rituals that are positive and perceived as pleasant, on the other hand, do not represent clinical compulsions.
It is generally recommended that people seek diagnostic work-up if they discover symptoms of obsessive-compulsive disorder and suffer from them. A diagnosis can be made by a doctor, psychologist, psychotherapist, or alternative practitioner. Psychologists, psychotherapists and specialists in psychiatry and psychotherapy in particular are trained to diagnose and treat mental illnesses such as obsessive-compulsive disorder. For this reason, it makes sense for those affected to turn to these professional groups. The family doctor can also be the first point of contact and, if necessary, issue a referral.
The subjective level of suffering is very individual in an obsessive-compulsive disorder. A strong subjective stress is also a reason to seek medical or psychological help. In addition, professional advice may be required if the compulsions lead to physical or other problems - for example, skin problems resulting from compulsory washing.
Doctors & therapists in your area
Treatment & Therapy
Early treatment of the Obsessive-compulsive disorder is recommended. First of all, the family doctor or a neurologist should be consulted, because damage to the brain regions can be treated with drugs that inhibit the absorption of serotonin. These are usually antidepressants or neuroleptics.
It also helps the person affected and their relatives to cope better with the obsessive-compulsive disorder when they seek therapeutic help. Conginitive therapy, in which the person concerned works towards the goal of changing their thought patterns, is very promising.
In this context, the sick person learns to deal with stressful situations, a suitable strategy for coping with everyday life and u. a. new behavioral patterns also in the interpersonal area.
You can find your medication here
➔ Medicines to calm down and strengthen nervesprevention
A Obsessive-compulsive disorder usually comes unexpectedly. However, if the sick person and their relatives find out more about the obsessive-compulsive disorder, recurrence is best prevented, but the obsessive-compulsive disorder should be accepted.
Aftercare
If the obsessive-compulsive disorder has been successfully treated and is no longer openly recognizable to others, it is now up to the person concerned to discover the first signs independently and immediately, if more suspicious, to seek a suitable (psycho) therapist in order to prevent a lengthy course of therapy. Furthermore, possible triggers, such as permanent, extreme stressful situations (also at work) should be avoided and instead your own behavior and thoughts should be checked regularly.
Even out of the affect, no casual, harmless habits for temporary calming should be developed, as these can later develop into an uncontrollable compulsion. However, if the compulsion is not cured and there is no prospect of a cure, it is essential for the person affected to accept his compulsion and, if possible, avoid places or other places where the compulsion cannot be controlled.
Not only with verbal compulsions, but also with thought or behavioral compulsions, it is advantageous to inform acquaintances and friends about your own behavior in order to prevent unpleasant situations or misunderstandings. Furthermore, the coercion - even in public - should not be violently overlooked, as this can not only cause a loss of control but also a strong discomfort on the part of the person concerned.
You can do that yourself
First, it's important to have a basic understanding of your OCD. This can make the situation easier for the person concerned. The person affected must be aware of how exactly his disorder makes itself felt and how it affects him and his life.
Also, it can be a great relief to know that you are not alone in your experiences. Those affected have to accept stress and learn to accept it not as a disruptive factor but as part of life. You should learn other strategies to deal with stress. For example, getting enough sleep, eating enough and good food, meditation, and getting enough exercise can all reduce symptoms. Running in particular can make a significant difference. Applying relaxation techniques (e.g .: deep breathing or meditative mindfulness exercises) is also helpful.
The next step would be to accept and confront his fears. Formulating negative thoughts about obsessive-compulsive disorder and proving them positively is proven to be an effective method for reducing the disorder and can also be used without therapeutic help. It often makes sense to deal with your fears in an analytical and logical way and to come up with strategies for the occurrence of the worst-case scenario. All of these techniques are easy to incorporate into everyday life and leisure.