As Acinetobacter baumannii is a dangerous hospital germ that is pathogenic to humans. The bacterium mainly affects people who have a weak immune system.
What is Acinetobacter baumannii?

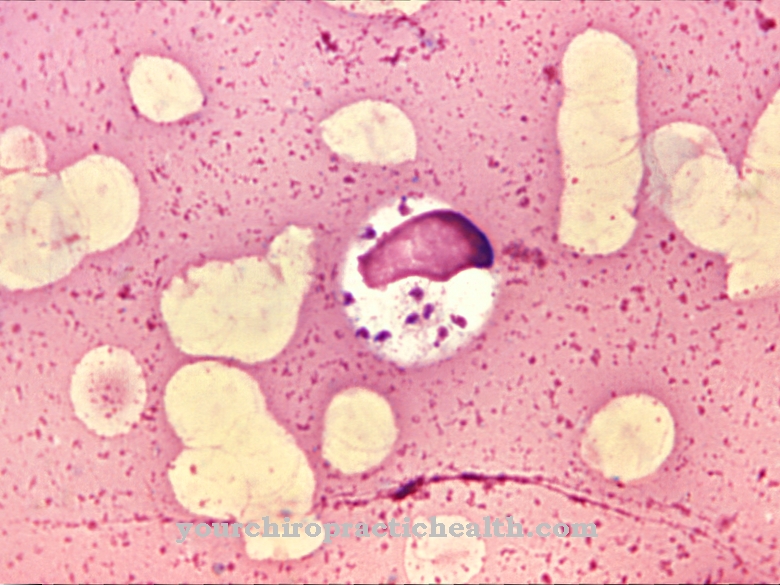
Acinetobacter baumannii is a gram-negative short-rod bacterium from the Acinetobacter group. It is one of the gamma proteobacteria and comes from the Moraxellaceae family. It also forms a new generation of hospital germs.
The Acinetobacter baumannii bacterium is considered to be of particular concern because it is resistant to antibiotics. It proves to be insensitive to four different groups of antibiotics such as cephalosporins, which come from the third and fourth generation, carbapenems, fluoroquinolones and acylureidopenicillins. As a result, common therapies with antibiotic active ingredients such as ciprofloxacin, ceftazidime, metropenem, imipenem, tazobactam, cefotaxime or piperacillin no longer have any effect.
It is not uncommon for people who previously had to undergo hospital treatment abroad to drag the resistant germs into German hospitals. How dangerous Acinetobacter baumannii is was shown at the beginning of 2015 at Kiel University Hospital. There, a total of 31 patients were infected with the pathogen, twelve of whom died.
Occurrence, Distribution & Properties
Acinetobacter baumannii is sometimes also Iraqi bacter called because the germ first attacked US soldiers between 2003 and 2004 who were stationed in Iraq and were injured in combat operations. The germ was also found in Bundeswehr soldiers who served in Afghanistan and suffered severe wounds. Over the years, Acinetobacter spread throughout the US and Europe and became a problem germ. In German hospitals, patients who previously had a hospital stay in Southeastern Europe, Eastern Europe, Southern Europe, Africa or Asia are classified as a risk factor. They threaten to introduce the multi-resistant bacteria. Too frequent use of broad-spectrum antibiotics is believed to be the cause of the spread of Acinetobacter baumannii.
The Acinetobacter baumannii bacterium is one of the environmental germs. The pathogen occurs on the one hand in water and soil and on the other hand on human skin or in the intestines. It is assumed that Acinetobacter baumannii forms part of their natural bacterial flora in around 25 percent of all people. The germ can also be found on plants as well as in insects and parasites. In addition, Acinetobacter baumannii is counted among the opportunistic germs. So its spread always takes place under the best conditions. This means that the bacterium prefers to settle in sick or injured people who already have a weak immune system. It is not uncommon for the affected people to be in the intensive care unit. Furthermore, infection from person to person is conceivable.
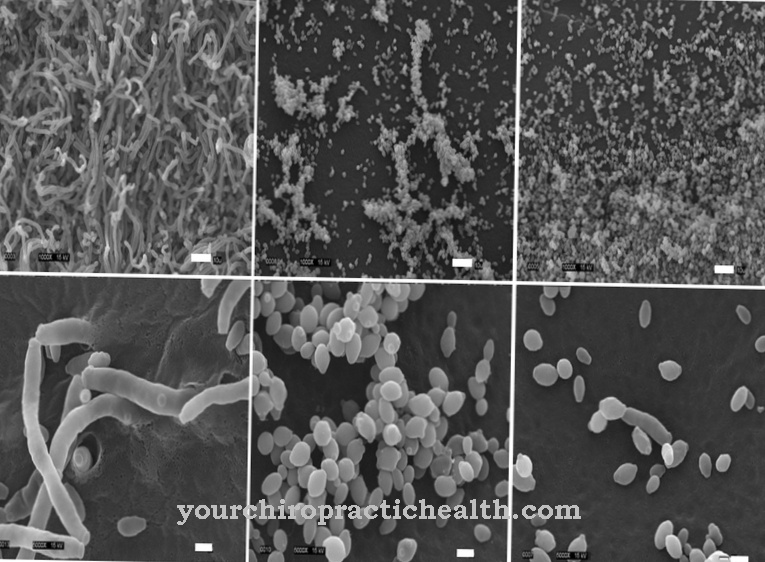
The name Acinetobacter is due to the fact that the bacterium is not endowed with flagella. Therefore, the germs are considered immobile. However, the bacteria do have the ability to move quickly on moist surfaces. The germs also form biofilms and are able to persist on surfaces for several weeks when dried out. These can be telephones, computer keyboards, or ventilators. Acinetobacter baumannii is usually transmitted in hospitals through the infected surfaces of medical devices or through the hands of the employees there. Transmission through the air may even be possible.
In addition to Acinetobacter baumannii, Acinetobacter nosocomialis and Acinetobacter pittii are also of clinical importance in Germany. However, the correct identification of the respective species is considered problematic, as the Gram staining of the bacteria is variable and therefore no reliable classification of the cocoid rods is possible. Biochemical processes also do not allow the germs to be identified at the species level. The result usually ends with a limitation in an ABC complex, which is clinically unsatisfactory. A reliable identification can now be made at least for Acinetobacter baumannii by a MALDI-TOF mass spectrometry.
You can find your medication here
➔ Medicines to strengthen the defense and immune systemIllnesses & ailments
If the person is healthy, Acinetobacter baumannii does not normally pose a threat. However, if the person is already very ill or has an immunodeficiency, there is a risk that the bacterium will lead to a hospital infection and severe pneumonia (pneumonia ) or blood poisoning (sepsis). Due to their severity, their course often leads to the death of the patient. People who are in the intensive care unit and are artificially ventilated there are considered to be particularly at risk.
Other diseases that can result from Acinetobacter baumannii are wound infections and urinary tract infections. Acinetobacter baumannii infection is additionally promoted by various risk factors. These include operations without antibiotic treatment, an ineffectiveness of the antibiotic and the use of medical instruments such as ventilators or catheters. Treatment of an Acinetobacter infection, which is usually done with reserve antibiotics, is very difficult.
Across the world, around 9 percent of all bacterial infections that occur in intensive care units are believed to be related to Acinetobacter. In Asia in particular, the disease rate is high at 19 percent. In Western European countries, the frequency of infection is around 6 percent. In Germany, two percent of all pneumonia is attributed to Acinetobacter baumannii.
However, it is possible to prevent the dangerous germ. Disinfecting, cleaning and isolating measures are particularly important. The thorough washing of the hands of doctors, nursing staff, patients and hospital visitors is of central importance. In the event of infection, the patient is strictly isolated. The patient may only be discharged after two different tests, in which Acinetobacter baumannii can no longer be detected.
Books about susceptibility to infections and immunodeficiency