The genus of bacteria Actinobacillus belongs to the department of proteobacteria and the Pasteurellaceae family. The name is related to the actinomycetes because the genus is often involved in actinomycoses as an opportunistic pathogen.
What is the Actinobacillus?
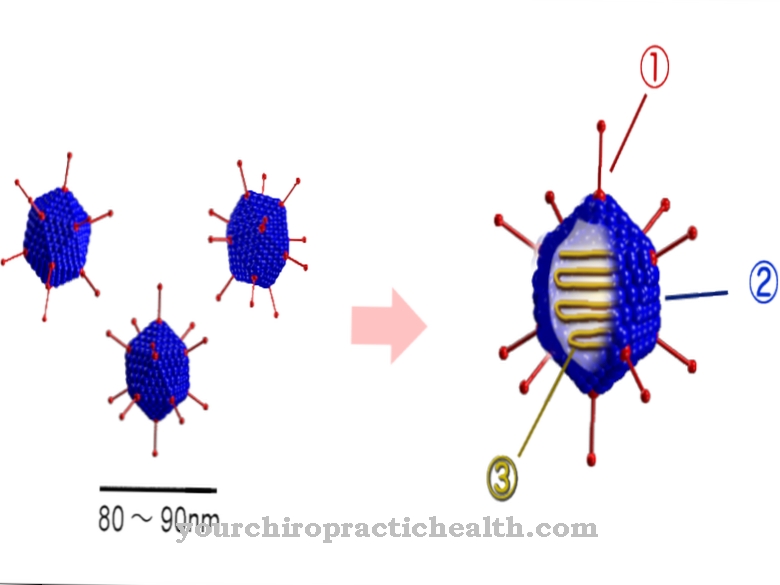
Bacterial species of the genus Actinobacillus have a slender and sometimes oval shape. They have no flagella and are immobile. The Gram staining is negative, so actinobacilli only have a murein shell with an overlying lipid layer.
Bacteria of this genus are facultatively anaerobic and can therefore survive very well in areas with little or no oxygen. Actinobacilli are not spore-forming and break down carbohydrates without producing gas.
Occurrence, Distribution & Properties
Actinobacillus bacteria have specialized in a parasitic way of life. They can parasitize mammals, birds, and reptiles.
A detailed analysis of Actinobacillus actinomycetemcomitans showed a monophyletic relationship to Haemophilus aphrophilus and Haemophilus segnis. A reclassification of the named species into the new genus Aggregatibacter ("aggregare" in the sense of "summarize, join together") is being discussed.
Illnesses & ailments
Germs from the genus Actinobacillus are accompanying germs in actinomycoses. Actinomycosis is a mixed infection caused by bacteria of the Actinomyzetaceae family. Pathogens of the genus Actinobacillus are not causative, but rather form part of the mixed infection as opportunistic pathogens.
The disease actinomycosis is referred to in German as "radiation fungus" because the focus of the infection was initially explained by a fungal colonization. Actinomycoses can also lead to fungal colonization, but since these are not to be regarded as the cause, the German term "radiation fungus" is misleading.
Actinomycosis is triggered by injuries to the mucous membranes. Resident actinomycetes of the normal bacterial flora penetrate deeper tissue layers through these injuries and trigger purulent inflammations here. Granulation tissue and widespread fistulas also develop.
The fistula formation is considered to be the main complication of the infection, since pathogens can enter the bloodstream and trigger a systemic infection. At the point of systemic infection, the prognosis for the patient is not good, as the systemic inflammation makes a high level of relapse (recurrence) even after an apparent recovery. A chronic illness cannot be ruled out even with timely antibiotic therapy.
A further complicating factor is that actinomycetes need several days of cultivation in order to be identified (about 14 days). PCRs also find it difficult to identify the causative pathogen in mixed infections.
The administration of antibiotics can ultimately lead to the causative germ being eliminated, but other germs with existing resistances to further drive actinomycosis. Given the complications and mechanisms of this mixed infection described, it is therefore not surprising that antibiotic therapy can last for a whole year and beyond.
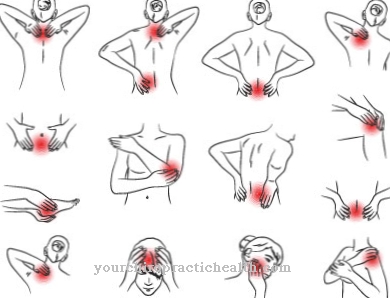
Cervicofacial actinomycosis, which is the term used to describe actinomycosis of the mouth, neck, and face, is the most common. Other forms of actinomycosis that extend into deeper layers of the skin or into the CNS are described less often. In principle, actinomycosis is possible in all positions on the body. Actinomycoses in the genital area and on the mammary gland have also been observed.
An exact diagnosis of the pathogen, including any resistances, takes place via the sputum. As an alternative, lung biopsies are also possible. The taking of tissue samples for direct detection of the pathogen is not promising.
An analysis of the sputum using the PCR method has so far been the best solution for identifying the pathogen. Antibiotic therapy can be started intravenously with aminopenicillin in the first three months. Tetracycline or cephalosporin are also suitable. A chronic infection with recurrent symptoms cannot be ruled out despite the fact that antibiotics have been administered for several months.
Bacteria of the genus Actinobacillus are still considered to be the cause of wound infections, endocarditis and bacteremia. A fatal course of the infection can occur especially in immunocompromised personalities. Here the mortality rate is around 30%. The wound infections caused only spread slowly and are mostly localized. Lymphadenitis can often be observed as an accompanying symptom.
Secondary infections, which can also occur after successful treatment and healing of the acute infection, play a further role. Serious late complications can primarily be caused in the central nervous system and the inner lining of the heart.
The germs Actinobacillus hominis and Actinobacillus urea play a special role for humans. Although the germs can also be found in the respiratory tract of healthy people, their involvement in the development of sinusitis, bronchopneumonia and meningitis is still controversial.
The Actinobacillus actinomycetemcomitans can also be found in the normal oral flora and is suspected to be responsible for the endocarditis together with other anaerobic organisms.
The germs of the genus Actinobacillus have not yet shown any pronounced resistance. Therefore, penicillin is used by default. In particular, the benzyl penicillins show good results in the treatment of Actinobacillus infections. The effectiveness of benzyl penicillins (Penicllin G) against gram-negative rod bacteria is unusual. The germs of the genus Actinobacillus are an exception here, which is useful for successful antibiotic therapy.
In the case of resistant germs, antibiotic treatment with ampicillin, tetracycline and cephalosporins can be continued. Identification of the causative agent is particularly important for effective treatment of existing infections. In the case of infections with strains of the Actinobacillus species, there can always be mixed infections and there is therefore the risk that some resistant germs are present.










.jpg)




.jpg)

.jpg)