The acute disseminated encephalomyelitis (ADEM) is a disease of the central nervous system (CNS). It is also called perivenous encephalomyelitis or as Hurst's encephalitis refers to and mainly affects children.
What is Acute Disseminated Encephalomyelitis?

ADEM belongs to the group of acquired demyelinating diseases of the CNS. A better known disease from this group is multiple sclerosis (MS). Acute disseminated encephalomyelitis is a rather rare disease. It manifests itself as an acute inflammation in the area of the central nervous system and often occurs one to four weeks after infection. In many cases, the symptoms resolve completely. However, damage can also remain. The disease is fatal only in rare cases.
causes
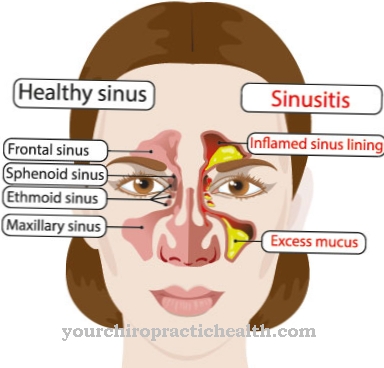
Acute disseminated encephalomyelitis is an autoimmune disease. In many cases the disease occurs after an infection. The causative infections include harmless upper respiratory tract infections, rubella, chickenpox, Epstein-Barr virus (glandular fever) or hepatitis viruses. Vaccinations can also result in ADEM.
It is also reported that ADEM can also be triggered by treatment with certain drugs or as a result of trauma. Cases without any triggering cause (idiopathic ADEM) are also known. A genetic background to the disease is discussed. Typical for the disease is an occurrence in winter and at the beginning of spring. It is believed that the inflammation in the central nervous system is caused by a cross reaction between brain proteins and pathogen components.
This means that in the infection that precedes ADEM, the body forms antibodies against the pathogens of this infection. These antibodies adhere to the pathogen and, together with other components of the immune system, ensure that the pathogen becomes harmless. In the event of a cross reaction, the antibodies that are actually directed against the pathogen react with the body's own cells. In ADEM, the antibodies attach to the nerve cells and to the myelin layer that surrounds the nerve cells.
The myelin layer plays an important role in the conduction of excitation in the nervous system. The binding of the antibodies to these cells causes an inflammatory reaction. So-called focal, i.e. focal-shaped, demyelinating foci occur. These are places on the nerve cords where the myelin layer is damaged. This damage can occur in the brain and spinal cord. They are often accompanied by swelling.
Symptoms, ailments & signs
Acute disseminated encephalomyelitis is characterized by a multitude of symptoms, which do not always have to occur. The symptoms depend on the localization of the damage. Overall, the symptoms are comparable to those of multiple sclerosis. However, while multiple sclerosis shows a relapsing course, the course of acute disseminated encephalomyelitis is limited to a single phase. In most cases, there is complete healing after the disease has passed.
In a few cases, however, there is only healing of the defect, in which individual symptoms persist after the disease has ended. In the context of acute disseminated encephalomyelitis, symptoms such as slowing of movements, impaired consciousness or even depression can occur.
Furthermore, it can lead to paralysis on one side, gait disorders, speech disorders, confusion or lethargy. The bilateral inflammation of the optic nerve, which leads to visual disturbances, is also characteristic of acute disseminated encephalomyelitis.
The beginning is often unspecific with fever, general feeling of illness, headache, nausea and vomiting. The disease progresses rapidly. Severe neurological failure symptoms can develop within hours of the onset of the uncharacteristic start.
Partial or complete paralysis can occur. If the respiratory muscles are affected by the paralysis, artificial ventilation is required. The patients often show meningism. Meningism is the painful stiff neck caused by irritation of the meninges. In addition to paralysis, gait or vision disorders can also occur.
Double images are characteristic. It can also lead to epileptic seizures. Some patients lose consciousness. Comatose states are also conceivable. Overall, the prognosis is rather favorable. In the majority of patients, the symptoms regress completely; defects only rarely remain. In rare cases, a particularly fulminant form of the disease, also known as Hurst's encephalitis, can occur. In this form of encephalitis, bleeding into the brain tissue occurs due to the death of blood vessels. As a result, the affected brain tissue often dies completely. Therefore, Hurst's encephalitis is often fatal.
Diagnosis & course
Various diagnostic methods are used if acute disseminated encephalomyelitis is suspected. Since computer tomography (CT) can only show larger lesions of the myelin layer, cerebral or spinal magnetic resonance imaging (MRT) is the method of choice. The MRI is used on the one hand to detect demyelination and on the other hand to rule out other diseases, such as multiple sclerosis. The follow-up is also carried out using MRI.
To confirm the diagnosis, the patient's cerebrospinal fluid, the cerebrospinal fluid, is also examined. Changes typical of the disease can be found here, such as an increased protein content or an increase in white blood cells, especially lymphocytes.
Complications
In the presence of acute disseminated encephalomyelitis, coma and syncope (loss of consciousness or fainting), headache, peripheral neuropathies (nerve damage to the peripheral nerve pathways, for example paralysis in the arms and legs) and ataxia (gross coordination disorder of muscle movements) are among the most common complications .
In addition to coma, delirium (confusion) and involuntary cramps all over the body (Kouristukset) are among the most visible neurological signs of disseminated encephalomyelitis. Other problems include optic nerve inflammation, myelitis (inflammation of the spinal cord) and manifested neuromyelitis optica.
If the disease progresses poorly, myelitis can lead to paralysis of the extremities, but also to complete incontinence (both urinary incontinence and fecal incontinence). If neuromyelitis optica has occurred, it can lead to loss of vision (up to complete blindness), headaches and impaired consciousness as well as seizures or spasms (convulsions).
Inflammation of the optic nerve can in turn lead to significant loss of vision. In addition to the fatal outcome of the disease, a coma with complete loss of consciousness is the most serious complication of acute disseminated encephalomyelitis. To avoid the complications mentioned or to alleviate the symptoms, an early and comprehensive diagnosis is the method of choice.
When should you go to the doctor?
Since the symptoms of this disease spread relatively quickly, a quick and immediate diagnosis and treatment is necessary to prevent further complications. A doctor should therefore always be consulted if there are lesions on the skin. These lesions are, in most cases, also accompanied by fever and nausea. Furthermore, those affected not infrequently suffer from headaches or vomiting. This disease can also lead to various disorders of sensitivity and paralysis.
Should this type of disorder occur or the person affected suffer from motor problems, a doctor must be consulted directly. Visual disturbances or hearing problems can also be symptoms of this disease. In the worst case, those affected suffer an epileptic seizure or even lose consciousness.
The hospital can also be visited directly or an emergency doctor called in the event of an acute emergency. General disorders of consciousness should also be examined by a doctor. Ideally, the examination should take place in a hospital in order to avoid further epileptic seizures, which could possibly lead to death.
Doctors & therapists in your area
Treatment & Therapy
Only a few studies exist for the treatment of acute disseminated encephalomyelitis, so that the treatment recommendations are based on empirical values. The patients are usually cared for in intensive care. In most cases, high-dose steroid therapy is used, i.e. various corticosteroids are used. Immunoglobulins are also administered.
If steroid therapy is unsuccessful, plasmapheresis is performed. During plasmapheresis, the blood plasma is exchanged. The liquid part of the blood is called blood plasma. This consists mainly of water, but other substances such as the antibodies that are responsible for acute disseminated encephalomyelitis are also dissolved in the blood plasma.
The patient's blood plasma is centrifuged and filtered using a plasmapheresis device. This is to remove the disease-causing antibodies circulating in the blood from the body. In individual cases, various immunosuppressants and cytostatics are also used to treat acute disseminated encephalomyelitis.
Outlook & forecast
Children are particularly affected by disseminated encephalomyelitis. In most cases, however, diagnosis is made late because the initial symptoms are not disease-specific and therefore do not indicate this disease. This leads to a severe fever and headache. The children also suffer from vomiting and severe nausea.
As the disease progresses, paralysis occurs in various areas of the body. The quality of life is considerably restricted and reduced by this paralysis. In addition to the paralysis of the body, eyesight can also be restricted and movement restrictions occur. It is not uncommon for those affected to suffer from epileptic seizures, which are also associated with pain. In severe cases it can lead to disturbances of consciousness and further loss of consciousness. The epileptic seizures should be treated immediately.
Often the parents and relatives of the patients also suffer from psychological stress or from depression and accordingly need treatment. Treatment of the disease itself is carried out with the help of drugs and blood plasma. This can severely limit the symptoms if early treatment is used.
prevention
Since the exact causes of acute disseminated encephalomyelitis are not yet fully understood, it is not possible to prevent the disease. However, the course can be favorably influenced by rapid diagnosis and rapid therapy. If a child has a fever again shortly after an infection and the affected child complains about visual disturbances, a doctor should be consulted immediately. The same applies to the occurrence of short "dropouts" or paralysis after an infection or a vaccination.
You can do that yourself
Since the disease primarily affects children, the self-help measures in everyday life are primarily to be implemented by adults and legal guardians. Medical care is necessary so that the symptoms can be alleviated. Self-treatment of the child is not recommended, as this can be expected to increase the number of irregularities.
To strengthen the physical as well as mental strength, various guidelines can be adhered to. It is important to strengthen the patient's immune system. The premises are to be supplied with sufficient oxygen. Outdoor stays are recommended whenever possible. The diet should be healthy and conscious. Vitamins and nutrients are necessary to support the body's immune system.
The sleeping conditions must be optimized so that the patient can recover sufficiently during night sleep or the necessary rest phases. Ideally, rest and wake phases should be adapted to the natural course and regulation should only be initiated when necessary.
To strengthen the psyche, positive elements must be embodied. Encouraging words and the promotion of fun and games are elementary building blocks of self-help. Family members should educate the patient in an understandable way about their condition while showing ways to improve it. Well-being is to be promoted by designing the environment, depending on the possibilities available.

.jpg)