The acute pancreatitis is a Inflammation of the pancreaswhich, in contrast to chronic pancreatitis, is mainly characterized by severe epigastric pain, nausea, nausea, constipation and fever. The first treatment measure for acute pancreatitis includes intravenous hydration and treatment with high-dose pain relievers.
What is Acute Pancreatitis?

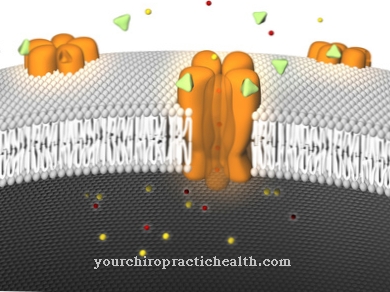
In acute pancreatitis, self-digestion occurs while digestive enzymes are released some time too early. The actual task of the released enzymes is to digest and utilize the nutrients such as proteins, fat and carbohydrates. However, since this process can take place before the ingestion of food, the organ digests itself.
Patients can suffer from this life-threatening disease several times, but in most cases they recover completely. Even so, acute pancreatitis leads to numerous complications.
causes
Acute pancreatitis can have many causes. Most of the time, however, the inflammation of the pancreas is due to gallstones. These are located in the duodenum for some time (this is also the mouth of the pancreatic duct).
As a result of this process, there is a backflow of the small intestinal juice and the bile acid simultaneously destroys the beginning of the pancreatic duct. These processes in turn lead to an increase in the permeability for certain phosphates and enzymes.
Another cause can be alcohol abuse, but it must be at least excessive or even chronic in order for it to lead to inflammation of the pancreas. The alcohol also triggers the processes described above.
In the remainder of the cases, no precise cause can be identified, which is why one speaks of these patients with idiopathic genesis.
Symptoms, ailments & signs
Acute pancreatitis is characterized by sudden severe pain in the upper abdomen. The pain is persistent and typically radiates to the back. In rarer cases, they also migrate to the chest. Often they encircle the body in a belt shape.
Furthermore, the abdominal wall is tense without becoming hard. This so-called rubber belly is characteristic of acute pancreatitis. These typical complaints can also be accompanied by nausea, vomiting, fever and flatulence. However, the intestinal noises are only weak, which indicates paralysis of the intestines and the danger of intestinal obstruction.
In severe cases it can even lead to a circulatory shock with a sharp drop in blood pressure, sweating, [[cyanosis9], thirst, kidney failure and a sharply increasing respiratory rate. If the pancreatitis is caused by gallstones or biliary tract disease, jaundice often develops, which is noticeable by the yellowing of the skin and greenish-colored dermis of the eyes.
At the same time, the stool will discolor and the urine will turn dark. In most cases, however, the acute pancreatitis is mild. Then it is only characterized by upper abdominal pain, which subsides after a few days. Complete healing takes place. However, if a large part of the pancreas is destroyed, the symptoms are very severe and the lethality is very high from circulatory shock, intestinal obstruction, organ failure or sepsis.
Diagnosis & course
In most cases, the first signs of acute pancreatitis are severe pain in the upper abdomen. These pains then radiate across the back so that the pain closes like a belt.
When examining the patient, clear symptoms of pancreatitis are a tender abdomen and a rubber belly. The rubber belly (also bloated belly) is caused by a large accumulation of gas in the gastrointestinal tract.
Also characteristic are only slight pain in the thoracic spine, which is very similar to the pain sensation in lumbago. However, this pain increases to the point of unbearable.
Other symptoms that are associated with the above, but sometimes do not appear until later, are constipation, nausea, vomiting and fever. Jaundice, ascites and signs of shock can occur in very severe cases of acute pancreatitis, among others.
Most cases are mild if treatment is started on time. Nevertheless, 20% of the illnesses are to be taken very seriously and in the most devastating case can lead to death.
Acute pancreatitis can have a mild and severe course. The most serious complications are deaths, for which up to 5 percent is given for the mild form and almost 100 percent for the most severe degree of the severe form.
Complications
In addition, a distinction must be made between complications directly related to acute pancreatitis and the long-term effects of this disease. The most serious complications directly related to pancreatitis are death from failure of the heart, lungs and kidneys. Bleeding associated with a drop in blood pressure up to shock, systemic inflammatory reactions, serious changes in the blood count and dehydration are observed.
Bleeding and accumulation of fluid in the abdominal cavity can lead to multiple organ failure; trypsin originating from the pancreas may attack the body's own organs. Breathing shallow from the pain can cause the lungs to collapse. Increased pressure in the abdomen and abdominal compartment syndrome may require surgical opening of the abdomen.
After an acute inflammation has been overcome, pancreatitis can recur at any time. The formation of pseudocysts and scar tissue can cause pain and be associated with infection, rupture and bleeding, and blockage of the bile duct can result, resulting in jaundice. The development of necrotizing pancreatitis with development of pus, liquefaction and tissue death is possible. So the complication of acute pancreatitis can be a chronic disease
When should you go to the doctor?
If acute pancreatitis is suspected, a doctor should be consulted immediately. Medical advice is required if you suddenly experience severe, belt-shaped radiating upper abdominal pain that cannot be attributed to any specific cause. If the symptoms persist longer than usual, a doctor's visit is necessary. An emergency doctor should be called in the event of severe complaints. A fever and sweating indicate severe inflammation of the pancreas, which can be fatal if left untreated.Even with sharp pain in the upper abdomen, there is an acute danger to life.
If the symptoms mentioned appear suddenly and increase rapidly, there is a high probability that it is acute pancreatitis that requires medical attention. Other contact persons are the gastroenterologist or internist. Anyone who regularly takes certain medications - such as diuretics, beta blockers or ACE inhibitors - should discuss the symptoms with the responsible doctor.
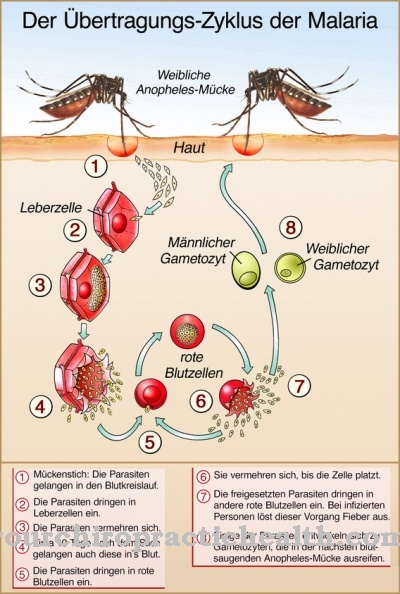
If the symptoms occur after a viral infection such as mumps, a worm infestation or a salmonella infection, this must also be clarified. Cancer patients and people with changes in their genetic makeup (hereditary pancreatitis, cystic fibrosis, etc.) should consult a doctor at the first signs of pancreatitis.
Doctors & therapists in your area
Treatment & Therapy
As soon as acute pancreatitis has been diagnosed, therapy should be started immediately. The first measure to be taken in the event of inflammation of the pancreas is usually intravenous fluids.
This is done to counteract an increasingly threatening volume deficiency shock, as this is caused by a significant loss of fluid. The fluids are usually accompanied by pain reliever therapy to stop the strong cramps. For a long time there was a belief in medicine that a certain diet could bring pancreatitis under control.
However, normal food can still be consumed in mild pancreatitis. In severe pancreatitis, which can lead to intestinal paralysis, a nasal and small intestinal tube is usually inserted early on so that nutrition only takes place through the intestines. If the acute pancreatitis is due to a jammed gallstone, it must be removed. Antibiotic therapy is usually also given to prevent infections.
Outlook & forecast
With pancreatitis there are various unpleasant symptoms. In the first place, the patient suffers from nausea with vomiting. There is also pain in the abdomen and a fever. These complaints can extremely restrict the patient's everyday life and thus significantly reduce the quality of life. Often, pancreatitis also leads to constipation and gas. In many cases, the stomach pain also spreads to the back.
In addition, if the disease is not treated promptly, jaundice can lead to liver damage. In the worst case scenario, the patient may die without treatment. Even if pancreatitis is diagnosed and treated late, organ damage can occur that is usually irreversible. As a result, the affected person can also die of organ failure or is dependent on a transplant.
In many cases, pancreatitis can be treated with pain relievers and antibiotics. Whether the disease progresses positively usually depends on the severity of the disease. Pancreatitis may reduce life expectancy.
prevention
Unfortunately, there are no preventive measures that can prevent acute pancreatitis. However, if the cause is excessive alcohol abuse, withdrawal can prevent further diseases from pancreatitis.
However, there are no effective preventive measures for stuck gallstones. In any case, the treatment measures should start as early as possible in order to prevent the worse development of acute pancreatitis.
Aftercare
Acute pancreatitis must be treated by a doctor, as it can lead to life-threatening complications. The patient is also asked for aftercare. Because many triggers of pancreatitis are related to unhealthy habits of the person affected.
Above all, alcohol and nicotine are to be mentioned as stimulant poisons, the avoidance of which in aftercare is a decisive factor for recovery, but also to prevent the disease from flaring up again. The family doctor and the treating internist will provide the necessary information.
Diet is another important factor in consistent follow-up care. The focus here is on a balanced diet. It helps to reduce high blood lipids, which are common in connection with pancreatitis and which can also promote other serious diseases of the cardiovascular and vascular system.
Avoiding flatulent, fatty, fried and cold foods is also important, as these can stress the pancreas in their function. If you are unsure which food and drink are suitable, you can find help from your family doctor, internist or dietician. Regular checks by the doctor are also important during aftercare and beyond. Follow-up appointments with the doctor must therefore be strictly observed in order to have blood values and functions of the internal organs checked professionally.
You can do that yourself
Immediate medical care is necessary in the case of acute pancreatitis. There are clear limits to self-treatment at home. In-house measures are highly recommended to accompany therapy or postoperatively.
After the stay in the clinic, those affected must continue to pay attention to a slow diet. The tolerance of vegetables, fish and meat should be tested slowly. Mostly there are digestive tract disorders. In order to support the body, care should be taken to ensure adequate hydration, and the food should be carefully chewed and well cooked.
Often those affected can only produce a few digestive enzymes. For this reason, fatty foods are poorly tolerated, which leads to flatulence and diarrhea. The missing enzymes can be replaced by a preparation. This should be taken with every meal. Furthermore, the consumption of nicotine and alcohol must be strictly avoided.
There is also a risk of developing diabetes mellitus due to the damage to the pancreas. In this case, sugar must be strictly reduced and a balanced diet with a high proportion of vegetables and fruits must be observed.
Regular exercise also stabilizes blood sugar levels and can compensate a little for what the pancreas is no longer capable of. If it is necessary to take insulin, it is advisable to visit a diabetologist at regular intervals in order to minimize the risk of further complications.

.jpg)

.jpg)



.jpg)


.jpg)






.jpg)
