A Nipple inflammation or breast infection is characterized by reddened and sore nipples and swelling of the breast. Depending on the severity of the infection, simple measures and rest are sometimes sufficient to bring about a rapid improvement. However, if the nipple infection is advanced, treatment with antibiotics or even surgery may be advisable.
What is a nipple infection?

© designua - stock.adobe.com
Mastitis or mastitis is an inflammation or infection of the breast, which can lead to severe swelling and pain, often accompanied by a fever. The infection is often caused or accompanied by inflammation of the nipple in question.
Mastitis can be caused, for example, by micro-injuries and the penetration of bacterial pathogens. Other causes can be hormone fluctuations, allergic reactions or abnormal tissue changes.
Both women and men can develop nipple infections. Most often, however, breastfeeding mothers are affected when they first start breastfeeding.
causes
The nipple (nipple) with the adjoining areola (areola) and the mammary glands (mammae) in the female body are sensitive areas of the body due to the numerous nerve tracts that end here. The breast and nipple are sometimes very sensitive to external or internal body-related irritations.
Since breast or nipple inflammation occurs most often, but not exclusively, in breastfeeding mothers, a distinction is made in the following text between breastfeeding-related mastitis and those nipple infections that are due to other causes.
Breastfeeding Causes:
If milk comes in shortly after birth or if a long time has passed between breastfeeding meals, one or both breasts can become overcrowded and swollen. Usually this uncomfortable state goes away quickly once the baby drinks. For various reasons, however, milk congestion can also occur, in which individual areas of the breast become hard and painful.
Causes for this can be, for example, too long breaks in feeding, mental or physical impairments of the milk flow reflex or injuries to the breast or nipple. If, in the case of a blocked milk, germs multiply in the blocked milk that have spread through a sore nipple or via the bloodstream in the body, a breast inflammation occurs through the formation of a painful abscess (pus focus). This inflammation often leads to inflammation of the nipple in question.
Other causes:
Injuries (abrasions or cuts) to the breast or nipple can also lead to bacterial infections in men. Bleeding or inflamed nipples are particularly common among long-distance runners. Due to frequent training and without the use of supporting functional underwear, as is the case with women, the textiles rub against the sensitive nipples and cause irritation and even inflammation.
Another cause that affects both women and men of advanced age is hormonal changes. During the menopause, the reduction in testosterone production leads to an increase in the level of estrogen in the male blood, which can also cause changes in the breast and nipple. Other changes in hormone levels, e.g. B. in puberty or cycle-related hormone fluctuations in women before menstruation or during the menopause are often the cause of tension, pain and inflammation.
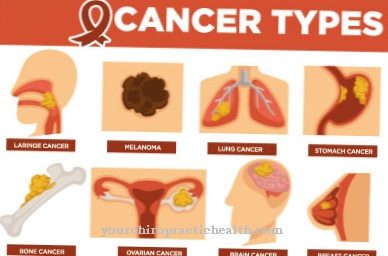
Furthermore, inflammation of the nipple can be caused by allergies or general intolerance to certain substances or chemicals (detergents, fabric softeners, cosmetics). Tumors in breast tissue are one of the most serious causes of nipple infections, although fortunately they are rare.
Symptoms, ailments & signs
Since the nipple is very sensitive, irritation shows up early in the form of redness, pain and increased pressure sensitivity. Inflammation of the nipple can occur on one or both sides, depending on the cause. The pain can radiate into the entire chest, which is then tense and hot and feels extremely painful when pressed.
The transition to the infection stage is shown by a fever of mostly over 39 °, which can be accompanied by a general feeling of fatigue, chills, sometimes vomiting and flu-like pain in the limbs. Breastfeeding mothers can also develop changes in breast milk secretion (bloody or purulent), crusts or discharge.
Other symptoms can include the formation of a purulent and palpable abscess or swelling of the affected lymph nodes. Incidentally, there may also be a discharge of secretion from the mammary gland that is not caused by breastfeeding, sometimes with blood or pus components. In any case, it is advisable to consult a doctor.
Complications
The transition between blocked milk and breast inflammation in breastfeeding women or nipple and breast inflammation for other reasons is fluid. Real mastitis is a dangerous complication that requires antibiotic treatment. Abscesses are considered a complication that, if not treated early enough, can worsen to such an extent that only surgical intervention brings relief.
When should you go to the doctor?
Breastfeeding mothers should immediately consult a midwife or lactation advisor if they develop obstructed milk or experience difficulties in breastfeeding. Often times, serious complications like abscesses can be prevented by acting quickly and vigorously. In any case, you should initially continue breastfeeding.
If there is no improvement within 24 hours, the indexing of an antibiotic should be discussed with a doctor.In general, even with nipple infections that are not caused by breastfeeding, the following can be said: If there is a fever and worsening pain, the progression of the infection should be prevented by a doctor.
If you are unsure about changes in the shape or color of nipples or if unclear secretions occur or if you feel lumps or abscesses, you should consult a doctor, as malignant, carcinoma changes in breast tissue can also be accompanied by such symptoms.
Doctors & therapists in your area
diagnosis
Regardless of whether the nipple inflammation occurred as a side effect of breastfeeding or due to other causes, the attending physician or midwife or lactation consultant will first palpate the breast concerned after a patient consultation and, if necessary, also examine it by ultrasound.
Abscesses and indurations can be identified quickly. If the secreted secretion is noticeable, a smear is taken and examined in a laboratory for pathogens and blood. If, on the other hand, the problem is suspected to be within the female milk ducts, a so-called galactography can be carried out. In this case, a contrast agent is introduced into the milk ducts by means of a probe in order to be able to display and examine them in detail on an X-ray image.
Further invasive and non-invasive examination methods can then be used to confirm the diagnosis, for example mammography is one of the most common breast examinations. Any tumors can also be detected with comparatively certain certainty. This examination method is therefore also part of the standard for early detection of breast cancer in women aged 40 and over.
If a suspicious lump or thickening is found during the examination, this change can be examined by means of a biopsy. In case of doubt and if there is a suspicion of a further illness, a blood and hormone test can provide additional information.
Treatment & Therapy
Since there are different causes of nipple inflammation, a specified treatment is also recommended.
In the case of a milk blockage and problems with breastfeeding, for example, cooling and gentle measures are often sufficient to bring about a rapid improvement. If in doubt, the measures should be discussed with a midwife or lactation consultant. For example, depending on the problems that arise, cold is advised to relieve pain and contain inflammation, and warm to dilate blood vessels.
For example, you can apply ice packs or cool compresses between breastfeeding periods. In acute cases, home remedies should also achieve very good results, for example chilled cabbage leaves, which when applied can quickly reduce the swelling and curb milk production somewhat. Quark or honey compresses or compresses with Retterspitz can also reduce the inflammation more quickly. In any case, breastfeeding should continue!
Not only do mother and child benefit from a longer breastfeeding relationship, the measure also helps the milk to drain off properly and prevents the inflammation from worsening. If those affected are open to homeopathic treatment, Phytolacca Cl 2 or Nux vomica C6 may help with congestion, and Belladonna C6, Hepar sulfur C6 or Silicea C6 help with breast inflammation. Bach flowers can also be used to provide relief, for example aspen, larch, mustard or crab apple.
If the nipple is particularly affected, herbal ointments can quickly provide relief. Preparations with ingredients such as wool wax and marigold ointment have shown the fastest improvements here. If there is no obvious improvement after treatment, drug treatment with antibiotics may be indicated.
In the worst case, if an abscess does not go away in any other way, only surgical measures will help. The pus abscess is opened as part of a small operation so that the pus can drain away.
Outlook & forecast
With a nipple inflammation - especially with breastfeeding-related diseases - literally every minute counts. The earlier an impending inflammation is recognized and the earlier therapeutic measures are started, the faster an improvement can be observed.
For example, if a blocked milk has been successfully cleared, the inflammation of breast tissue can be prevented in most cases. If there is inflammation, the household or herbal remedies described usually help within a few days. If antibiotics are administered, a few weeks should be enough for the inflammation and its accompanying symptoms to heal successfully and completely.
However, the prognosis for untreated inflammation is rather poor. The formation of purulent abscesses through to the formation of indurations, skin rashes or, in rare cases, malignant tumors, required a comparatively lengthy therapy, which often also necessitated surgical interventions.
prevention
Even before breastfeeding, you can prevent nipple and nipple infections. It has been observed that heat is effective here. For this you can either place a warm, damp cloth on your chest or simply take a warm shower more often. A tip among midwives is also a potato wrap just before breastfeeding.
For this, warm jacket potatoes are wrapped in a kitchen towel, crushed and the towel is placed around the breast concerned. Alternatively, poultices made from powdered fenugreek seeds, mixed with hot water to form a pulp, can help. Like potatoes, this seed contains an anti-inflammatory component and prevents the breast tissue from becoming inflamed in the first place.
In general, strict hygiene should be observed during breastfeeding. Regularly changing the nursing pads is recommended. The right breastfeeding technique also has a decisive influence on the good flow of milk. A midwife or lactation consultant will be happy to provide advice and assistance. The cost of postpartum care is usually borne by the health insurance company. You should therefore look to a midwife early on and during pregnancy.
To prevent inflammation of the nipple caused by allergic reactions, you should pay attention to skin irritations after changing cosmetics or detergents and replace them if necessary. The same applies when wearing certain fabrics or textiles. Many people complain of skin irritation when using synthetic fabrics. Often it helps to wear a garment made from natural fibers under the synthetic garment. To prevent bleeding and inflamed nipples caused by chafing, endurance athletes are best able to tape their nipples with a plaster before training and competitions.
Aftercare
After a nipple infection, it is imperative to take follow-up measures. Otherwise it will quickly lead to renewed inflammation. The earlier you recognize their signs, the easier it is to avoid a painful infection. If the nipple inflammation occurs increasingly during breastfeeding, it is advisable to change the breastfeeding method and breastfeed more often.
During the breastfeeding breaks, the sensitive areas of the skin can either be treated with cold for relief and to reduce swelling, or with warmth the vessels can be expanded and the blood circulation promoted. Old home remedies such as cold quark compresses or warm potato compresses are suitable for this. Herbal ointments like marigold ointment have also been shown to be good prevention.
If the nipple inflammation is allergic, you should change detergents and cleaning agents and possibly investigate the cause of the intolerance of certain cotton blends. A different, hypoallergenic detergent or a change in the cotton content of tops is often sufficient to completely prevent recurring nipple infections.
Athletes can wear functional underwear to protect the textiles from rubbing against their skin or mask sensitive areas with plasters before training. Medical follow-up care after a nipple infection is usually not required. However, if you observe the preventive measures, another infection can be avoided, or usually alleviated without antibiotic treatment.
You can do that yourself
Those affected can help themselves, especially with breastfeeding-related inflammation of the nipples. Above all, you should allow yourself some rest. Life with a baby turns everything that has gone before on its head and demands a lot from the body and mind of the young mothers. It often helps to just lie down in bed with the child for a day or two and relax.
The designation of the first weeks after the birth as “childbed” also makes the profound change in everyday life clear in language. At least one should try to pedal a little slower for at least a few days. Midwives often advise keeping the breast empty when breastfeeding problems occur. If necessary, you should breastfeed at least every one to two hours so that the breast in question does not fill up too much. If only one side is affected, the child should always be placed on that side first so that it is safely emptied.
The right breastfeeding technique is also important. A midwife should help with donning and breastfeeding if anything is unclear or if you have any questions. For breastfeeding mothers, it is generally advisable to avoid incisive and restrictive clothing. Often there are psychological insecurities and problems behind breastfeeding problems. In this sensitive situation, it is therefore particularly important to talk to a lactation consultant or midwife.


.jpg)








.jpg)

.jpg)
.jpg)











.jpg)