The acute cholinergic syndrome is characterized by increased stimulation of the vagus nerve. The cause of this stimulation is an increased concentration of acetylcholine, which acts as a neurotransmitter in the parasympathetic nervous system. Acute cholinergic syndrome is treated by blocking the muscarinic acetylcholine receptors with atropine.
What is Acute Cholinergic Syndrome?

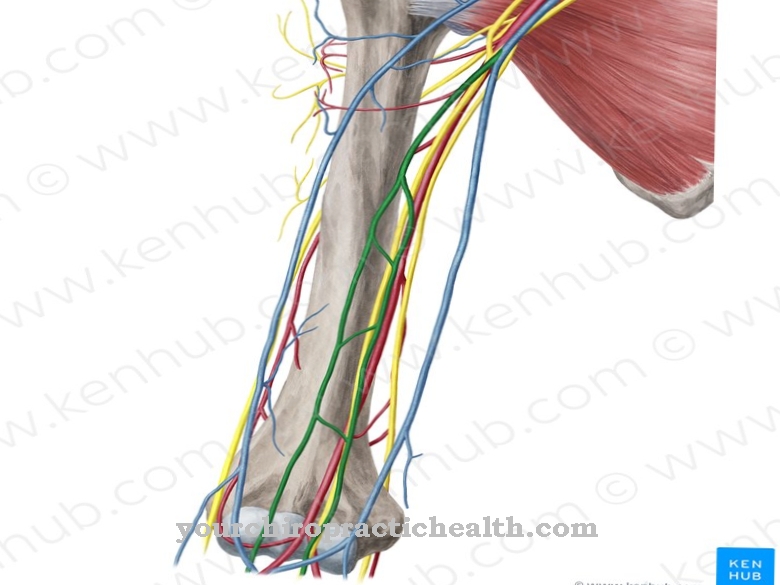
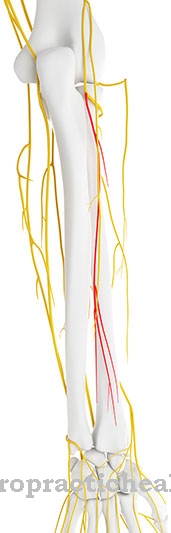
The acute cholinergic syndrome is an overstimulation of the vagus nerve. The vagus nerve is part of the parasympathetic nervous system, which is responsible for the function of the internal organs. The parasympathetic nervous system is stimulated by the neurotransmitter acetylcholine. For this purpose, acetylcholine binds to the nicotinic or muscarinic acetylcholine receptors of the nerve cells.
In addition to acetylcholine, nicotine can dock with the nicotinic acetylcholine receptors. Accordingly, the mushroom poison muscarin, which is found in the fly agaric, for example, can bind to the muscarinic acetylcholine receptors. In the acute cholinergic syndrome there is an oversupply of acetylcholine, which leads to the corresponding symptoms via the binding to the muscarinic acetylcholine receptors of the vagus nerve.
The vagus nerve is the tenth cranial nerve. It is responsible for regulating almost all internal organs. In Latin there is the word "vagaris", which means something like "to wander around". Hence, the term vagus nerve means in translation the "wandering nerve". It innervates various organs to control their motor or sensitive function.
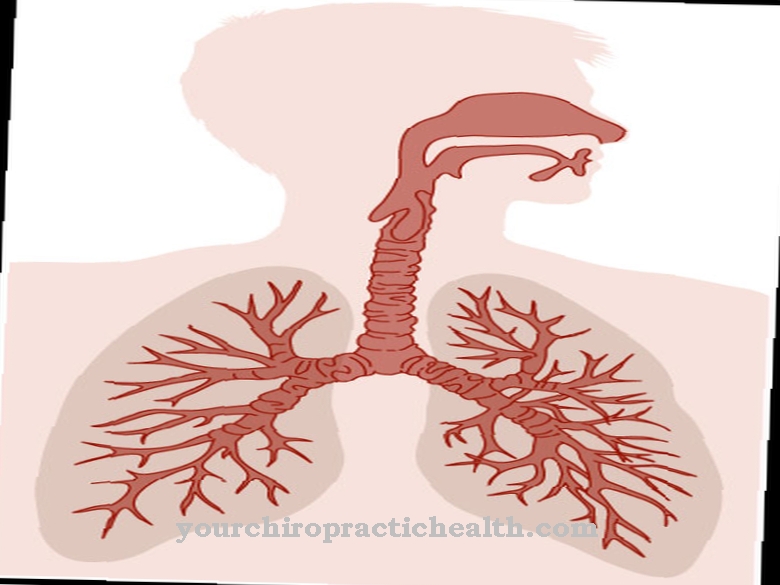
It has a particular influence on the involuntary control of the motor functions of the larynx, throat and esophagus. It also conveys the taste sensations of the tongue or touch sensations in the throat, in the external auditory canal or on the larynx. In the chest and abdomen, the vagus nerve is responsible for mediating reflexes.
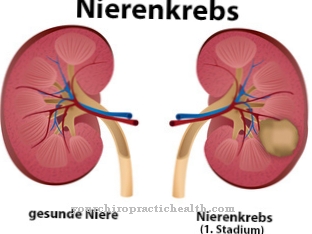
This affects the heart, lungs, windpipe or esophagus in the chest. In the abdomen, the stomach, pancreas, intestines, gall bladder, liver and kidneys are stimulated. Therefore, in acute cholinergic syndrome, these organs are overstimulated.
causes
Since the neurotransmitter acetylcholine is responsible for stimulating the internal organs, too much acetylcholine must be present in an acute cholinergic syndrome. Acetylcholine is broken down into choline and acetic acid with the help of the enzyme acetylcholinesterase after it is released in the synaptic gap.
However, if the effectiveness of the enzyme is suppressed, this degradation can no longer take place sufficiently. Acetylcholine accumulates in the synaptic cleft. It binds itself to the acetylcholine receptors, which then begin to transmit signals between the individual nerve cells of the vagus nerve.
The enzyme acetylcholinesterase can be deactivated, among other things, by certain organophosphorus compounds. These organophosphates bind irreversibly to the active center of the enzyme. These substances include the nerve toxins tabun and sarin or the pest control and plant protection agents malathion and diazinon.
The chemotherapeutic agent irinotecan also inhibits the enzyme acetylcholinesterase. The same goes for the drugs neostigmine and physostigmine. Both of these drugs are reversible inhibitors of acetylcholinesterase. This means that the active ingredients bind to the enzyme, but can be split off again.
Overall, it can be said that the acute cholinergic syndrome is a poisoning syndrome. The effects of these poisons are different. The nerve toxins tabun and sarin were used as warfare agents. They are fatal within seconds, while other acetylcholinesterase inhibitors produce milder symptoms.
Symptoms, ailments & signs
Acute cholinergic syndrome is characterized by the symptoms of diarrhea, sweating, increased salivation, watery eyes, abdominal pain, narrow pupils with visual disturbances, drowsiness, dizziness, malaise, chills, conjunctivitis and low blood pressure due to vasodilation.
All symptoms are an expression of the motor and sensitive overstimulation of the internal organs. At best, these are side effects when using certain drugs. Organophosphorus compounds can, however, cause massive poisoning, which in the case of the nerve toxins tabun and sarin often lead to death within seconds.
Diagnosis & course
The diagnosis of acute cholinergic syndrome is based on anamnesis of the medical history. The compilation of the typical symptoms can lead to a suspected diagnosis. It also analyzes which drugs were administered in which concentration. In addition, in this context it can also be asked which substances the person concerned has come into contact with.
Complications
The tenth cranial nerve, known as the vagus nerve, is responsible for regulating a large number of internal organs. Patients suffering from acute cholinergic syndrome have overstimulation of this cranial nerve, which causes immediate disorders of the affected organs in the chest and abdomen. This overstimulation affects the heart, liver, lungs, esophagus, and trachea in the chest.
In the abdomen, the pancreas, stomach, intestines, liver, gallbladder and kidneys are affected. The acute cholinergic syndrome has a particular influence on the control of motor functions in the pharynx, the esophagus and the larynx. The multiple organic disorders cause diarrhea, tears, increased salivation and abdominal pain.
Low blood pressure, muscle cramps and dilated blood vessels are also typical. These symptoms are treated with the neurotoxin atropine. This has the opposite effect, which leads to the blockage of the parasympathetic nervous system. This blockage is known as anticholinergic syndrome. Through therapy with atropine as an antidote, the multiple organic disorders are eliminated.
Since in most cases this poisoning syndrome is due to drugs that act directly on the autonomic nervous system, patients receive a positive prognosis. Complete healing usually occurs after a short period of treatment. Treatment must be carried out soon after diagnosis, otherwise serious complications can occur.
When should you go to the doctor?
With this syndrome there are many different complaints. As a rule, a doctor should always be consulted. Since symptoms usually occur after taking certain medications, they must either be stopped or replaced with other medications. However, this should only be done after consulting a doctor. Those affected suffer from malaise, drowsiness and confusion.
The resilience of the person affected is also considerably restricted and visual disturbances or diarrhea can occur. If these complaints occur for no particular reason, a doctor must be consulted in any case. Medical help is also necessary if you have low blood pressure or loss of consciousness.
If there is a loss of consciousness, the emergency doctor can also be called. It is not uncommon for the internal organs to be affected by this syndrome. If there are problems with the kidneys or the heart, urgent treatment of the patient is also necessary. In acute emergencies, you should always go to a hospital or call the emergency doctor.
Doctors & therapists in your area
Treatment & Therapy
Acute cholinergic syndrome is mainly treated with atropine. Atropine is actually a poison that blocks the effects of acetylcholine. It binds to the muscarinic acetylcholine receptor and thus displaces acetylcholine from this place.
With a significant concentration of atropine, the opposite anticholinergic syndrome occurs, which is characterized by the blockage of the parasympathetic nervous system. However, when the concentration of acetylcholine is increased due to the inhibition of acetylcholinesterase, atropine acts as an antidote, preventing the symptoms of acute cholinergic syndrome.
With the very strong organophosphorus neurotoxins such as tabun or sarin, the treatment is often unsuccessful because these substances bind irreversibly to the enzyme and thus block it. Mainly, however, it is poisoning caused by overdosing with cholinergic drugs, which respond much better to treatment with atropine.
In addition to atropine, the active ingredient midazolam is also administered for muscle cramps. This substance from the group of benzodiazepines increases the effect of the neurotransmitter gamma-aminobutyric acid (GABA). If acidosis is still the symptom, sodium hydrogen carbonate is given to neutralize it.
Outlook & forecast
With this syndrome, patients usually suffer from various ailments. In most cases this results in watery eyes and severe diarrhea. Increased sweating and salivation are also common symptoms. Abdominal pain and drowsiness can also occur in the patient. Those affected feel uncomfortable, tired and sick. There is a chills and not infrequently dizziness.
The affected person can also lose consciousness due to the reduced blood pressure. A fall can result in injury. It is not uncommon for this syndrome to also lead to conjunctivitis. In very serious cases, the poisoning can lead to death of the patient after just a few minutes.
The symptoms of this syndrome can be treated with the help of medication. Under certain circumstances, however, the internal organs are irreversibly damaged by the poisoning. A universal prediction about the course of the disease is not possible in this case. As a rule, however, rapid treatment does not lead to further complications or to a reduction in life expectancy.
prevention
To prevent acute cholinergic syndrome, overdosing should be avoided when administering cholinergic drugs.
Aftercare
As a rule, the person affected with this syndrome has very few or even no measures and options for follow-up care available. The person concerned is primarily dependent on the rapid and, above all, early diagnosis of the syndrome so that there are no further complications or complaints.Only with early detection of this disease can further complaints be avoided.
Therefore, early diagnosis is paramount in this syndrome. The person concerned is dependent on inpatient treatment for this disease, which usually takes place in a closed institution. Furthermore, the person affected is often dependent on the care and support of their own family or friends in order to make everyday life easier.
Intensive and loving discussions are also very important in order to prevent depression and other psychological upsets. It is also necessary to take the antidote to alleviate the symptoms. The person concerned should ensure the correct dosage and regular intake. Whether this syndrome will lead to a reduced life expectancy cannot be universally predicted.
You can do that yourself
The acute cholinergic crisis is a medical emergency. The person concerned or a first aider must alert the emergency doctor and ensure that the doctor is informed immediately about possible causes. If the symptoms occur immediately after taking medication or any toxins, the doctor should be informed. In addition, the patient should lie on their back and not move until medical help arrives.
Artificial vomiting should only be done under the supervision of a professional. If you have severe abdominal pain or a fever, use home remedies such as cooling pads or green tea. Medication should not be taken during an acute cholinergic crisis. The condition requires inpatient treatment.
Then the patient should take it easy and, if necessary, change their diet in order to promote recovery. The triggering drug or poison must be identified and avoided. The patient should contact the doctor for this and, if necessary, also consult a nutritionist. If, despite all measures, signs of an acute cholinergic syndrome appear again, the responsible doctor must be informed immediately.

.jpg)
.jpg)

.jpg)


.jpg)













.jpg)