Aldosterone is one of the steroid hormones and is responsible for the body's water and mineral balance. It retains more water and sodium ions in the body, while potassium ions and hydrogen ions (protons) are excreted. Both an aldosterone deficiency and an aldosterone excess lead to serious health problems.
What is aldosterone?
Aldosterone is a steroid hormone made by the adrenal glands. It is also known as the thirst or salt hormone because it significantly controls the body's water and salt balance. The hormone is a mineral corticoid, which belongs to the group of corticoid steroids. Its production takes place in the adrenal cortex, along with other steroid hormones such as cortisol and sex hormones.
Blood pressure is regulated with the help of aldosterone. If the blood pressure falls, there is an increased release of aldosterone. When blood pressure rises, the synthesis of aldosterone decreases. This regulating mechanism is mediated by the renin-angiotensin-aldosterone system. As part of the renin-angiotensin-aldosterone system, the body's mineral and water balance is regulated depending on external influences. A high water and salt loss reduces the excretion of urine by the kidneys and at the same time increases the feeling of thirst and the hunger for salt in order to restore the balance. Aldosterone plays a central role in this system.
Anatomy & structure
As already mentioned, aldosterone is a steroid hormone. Steroid hormones have the same chemical structure as cholesterol. Thus, cholesterol is also the starting molecule for the production of aldosterone and the other steroid hormones. Pregesterone is formed through oxidation via the intermediate pregnenolone from cholesterol.
After further hydroxylation of Pregesterone and subsequent oxidation of the hydroxyl groups, aldosterone is finally formed. Its production takes place in the outer layer of the adrenal cortex, the zona glomerulosa. Its synthesis is triggered as a result of a reduction in blood volume and blood pressure or an excessively high potassium concentration (hyperkalaemia) in the blood. Angiotensin II, which forms within the framework of the renin-angiotensin-aldosterone system, acts as a mediator of the synthesis.
When the sodium concentration in the blood increases, the biosynthesis of aldosterone is inhibited. This increases the concentration of the atrial natriuretic peptide (ANP) and flushes out sodium by increasing the urine output. The regulating hormone ACTH in turn stimulates the production of aldosterone.
Function & tasks
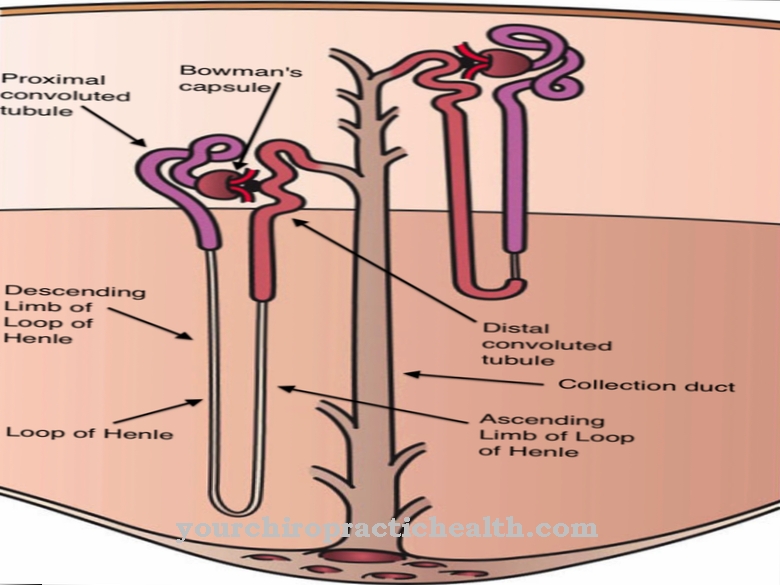
Aldosterone has the function of regulating the body's water and mineral balance. It serves to maintain the physiological relationship between potassium and sodium ions in the blood. The hormone increases the incorporation of sodium channels (ENaC) and sodium transporters (Na + / K + -ATPase) into the plasma membrane of the epithelial cells of the kidneys, lungs and colon.
These sodium channels are permeable to sodium ions and thus cause sodium to be reabsorbed from the primary urine or the intestinal lumen. At the same time, the excretion of potassium and ammonium ions as well as protons increases. This leads to an increase in the extracellular volume, a decrease in the potassium concentration and an increase in the pH value in the blood. Aldosterone is a hormone that can develop its effectiveness via a corresponding receptor in the cell membrane. Certain aldosterone antagonists such as spironolactone or eplererone can inhibit the effects of aldosterone by blocking the receptor.
Cortisol, like aldosterone, also binds to the mineral corticosteroid receptor. This is why it is oxidized to cortisone in the intestines, kidneys, or some other tissues. In this form it can no longer bind to the receptor. As a result, it loses its antidiuretic effectiveness, but continues to perform its tasks as a stress hormone separately from this function. However, this no longer hampers the excretion of toxic substances with the urine. The regulation of aldosterone takes place via the renin-angiotensin-aldosterone system.
As part of this system, if there is a drop in blood pressure or a loss of water or sodium, the enzyme renin is initially released from specialized parts of the kidney tissue. Renin in turn causes the formation of angiotensin II via the intermediate stage angiotensin I. Angiotensin II increases the blood pressure by narrowing the fine blood vessels. At the same time it stimulates the production of aldosterone, which causes the reabsorption of sodium and water.
Diseases
Both a deficiency and an excess of aldosterone can lead to significant health problems. With an aldosterone deficiency there is an increased excretion of sodium and water. Symptoms include low blood pressure, tiredness, confusion, vomiting, diarrhea and cardiac arrhythmias. The level of potassium in the blood is too high.
Newborns with aldosterone deficiency are referred to as salt loss syndrome, with poor drinking with refusal to eat, vomiting, diarrhea, dehydration and increasing indifference occurring in the first days of life. The disease is life-threatening and must be treated immediately. There is both primary and secondary aldosterone deficiency.
The primary aldosterone deficiency is due to a disease of the adrenal glands. In extreme cases, the so-called Addison's disease can develop with total failure of the adrenal cortex. In addition to aldosterone, the other steroid hormones are also missing here. The secondary aldosterone deficiency, in turn, is due to a faulty regulatory mechanism in the renin-angiotensin-aldosterone system.
Treatment of aldosterone deficiency is through hormone substitution and treatment of the underlying disease. The overproduction of aldosterone can also have primary or secondary causes. The primary overproduction of aldosterone is usually caused by benign or, more rarely, malignant tumors in the adrenal glands.
The primary form of overproduction is Conn's syndrome, which manifests itself in muscle weakness, headache, thirst and frequent urination. The secondary aldosterone overproduction shows similar symptoms and is caused by a dysregulation in the renin-angiotensin-aldosterone system, as is the case with secondary aldosterone deficiency.