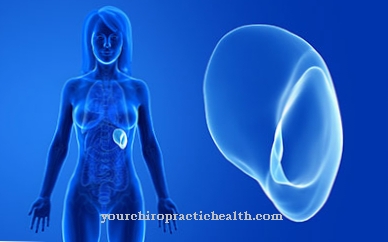
As Anal atresia is a malformation of the human rectum. The opening of the anus is missing or not correctly positioned.
What is anal atresia?

Doctors also call an anal atresia one Anorectal malformation. What is meant is a malformation of the rectum that has existed since birth. There is no breakthrough in the anal pit within the rectum. In an embryo, this normally takes place over a length of 3.5 centimeters.
Anal atresia affects about 0.2 to 0.33 percent of all newborns. In Germany, the anorectal malformation occurs every year in 130 to 150 babies. In most cases, the anal atresia is diagnosed shortly after birth. The malformation of the rectum is more common in male children than in girls.
causes
In the case of anal atresia, the rectum does not form on the body part that is intended for it. This can lead to a blind end of the bowel or a transition into a fistula. The latter opens into the bladder, urethra or the female vagina. A forward shift on the pelvic floor is also possible.
What causes the anal atresia has not yet been found out. Genetic factors are primarily suspected to be the trigger. The risk of anal atresia in siblings of children who already suffer from the malformation is 1: 100, as far as the lighter forms are concerned. For the other forms, the probability is between 1: 3000 and 1: 5000.
Studies have shown that two-thirds of all children with anal atresia have additional abnormalities. 15 percent of all sick people also suffer from genetic defects. These include, in particular, Down syndrome, Pätau syndrome and Edwards syndrome.
Symptoms, ailments & signs
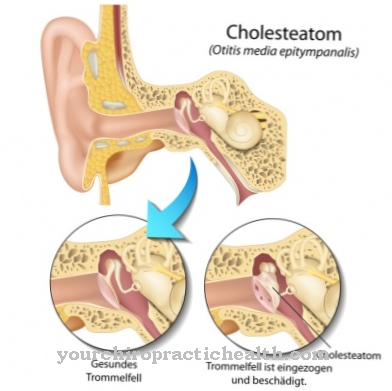
Anal atresia can be divided into several forms. Most of those affected develop different fistulas. Boys often suffer from anal atresia with a recturethral fistula. In contrast, girls usually have a rectovestibular fistula that arises between the atrium of the vagina and the rectum. Other forms of fistula in boys are the anouctane, anopenile, anoscrotal, rectovesical, rectoprostatic and rectoperineal fistula.
Anocutaneous fistulas and ectoperineal and rectovaginal fistulas also occur in women.Sometimes anal atresia is classified according to the level of the malformation. A distinction is made between high, low and intermediate forms. The higher the anal atresia, the greater the risk of additional malformations in other parts of the body.
A distinctive feature of anal atresia is the lack of the anal opening at the anus. Sometimes fistulas are also noticed after the birth. In some cases, stool or air is evacuated through the female vagina or urethra. A bloated stomach can also be a noticeable symptom. Further malformations are found in 50 to 60 percent of all sick children. The urinary region is particularly affected. In addition, malformations of the gastrointestinal tract, the spine or the heart often occur.
Diagnosis & course
It is not possible to reliably determine anal atresia before birth as part of the prenatal diagnosis. There is only the option of diagnosing accompanying malformations. Even with an ultrasound scan, anal atresia is difficult to identify. In most cases, the anorectal malformation is noticed by the absence of the anus or because the stool is leaking in a place not intended for it.
Following the first finding, a perinaeal ultrasound examination takes place. In this way, the distance between the target point of the anus and the rectum blind sac can be determined. If anal atresia is diagnosed early, it can be treated well in most cases. Social continence can also be achieved with careful follow-up care. At a young age, those affected are usually able to control social continence much better.
Complications
Anal atresia is a rather rare embryonic malformation. With this symptom, either the rectum and anus may be misplaced or not formed. So far there are no exact causes for the development of anal atresia within the embryonic development. The malformation affects boys more than girls and has additional variable fistulas.
The infants affected sometimes show other genetic anomalies, such as Down syndrome. A wide range of complications will accompany the child for a lifetime. Infants with anal atresia are examined thoroughly immediately after birth. The severity of the symptom and any other accompanying malformations are diagnosed.
The medical measure is only initiated after the findings have been taken. Surgical correction of anal atresia takes place in the first nine months of life. In the case of a severe form of the malformation, an artificial anus and the actual anus are first placed and then brought together a little later. In the simplest case, the complete correction can be carried out immediately.
The surgical procedure enables relative continence. The affected children can often only learn to control them better in their adolescence. The extent to which continence can be fully or only partially restored depends on the degree of the malformation. Some of the patients suffer from psychological and physical secondary damage. You need a lifelong treatment plan and regular check-ups.
Treatment & Therapy
Treatment of anal atresia must always be performed surgically. There are differences in therapy when a fistula is present. If there is a fistula, the height of the malformation and its position play a decisive role. In addition, it is important to clarify whether the creation of an artificial intestinal outlet is necessary before the corrective procedure. With a metal rod, a fistula can be widened towards the perineum without any problems.
If there is no expansion of the intestine, there is no need for an artificial anus. This is necessary when the stool emerges through the urine or the vagina.
If there is no fistula and the distance between the skin and rectum is less than one centimeter, the surgical correction of the anal atresia takes place without a colostomy. If the distance is longer, an artificial intestinal outlet is created first. In the operation, known as posterior saggital ano-recto-plasty (PSARP), the surgeon loosens the stump of the rectum that does not open in the external direction and, if necessary, closes an existing fistula.
Then the intestinal stump is opened. The surgeon also uses a suture to create an anus on the outside. An artificial anus is later closed again so that the continuity of the intestine can be restored. As part of follow-up care, the child's parents have to regularly expand the newly created anus with a metal rod for a year.
Doctors & therapists in your area
Outlook & forecast
Thanks to modern surgical methods, anal atresia can usually be corrected well, provided it is performed in good time. The required operation usually leaves hardly any damage, with the extent of any subsequent complications being determined by the form of the anal atresia. Frequently existing fistulas between the intestinal tract and internal organs or the outside of the body are also decisive for the course of the operations.
An artificial anus or a correction of the anus using existing tissue usually leads to a functional bowel. If nutritional and intestinal care measures are observed, complications that occur - especially incontinence and constipation - can be reduced or prevented. If the pelvic floor muscles and intestines are exercised, the prognosis for faecal incontinence is good overall.
The extent of the agenesis (the absence) of other body parts in the lower trunk area often determines the long-term prognosis. Missing or improperly formed parts of the spine occur in approximately half of all people with anal atresia. The long-term prognosis is based on the resulting suffering and physical limitations. Since this form of malformation almost always occurs as a symptom of an illness - usually a syndrome - the symptoms of the respective illness must also be taken into account for the prognosis.
prevention
Since the causes of anal atresia are not known and it is a congenital malformation, there are no effective preventive measures.
Aftercare
Analresia is usually treated surgically. As a result, the typical complaints usually do not recur. Patients only need to see a doctor several times immediately after an operation. This monitors the healing process. Medicinal support also takes place.
There is no long-term follow-up in the event of a positive surgical intervention. Anal resia cannot be prevented in advance. It is congenital and is mostly diagnosed in young children. A physical examination is sufficient to determine this. An x-ray and an MRI will be arranged regularly.
Follow-up care may be necessary, especially during puberty, with regard to the mental state of those affected in order to reduce psychological stress. Because despite extensive continence, patients describe small smears in their underwear. Psychotherapy can help to learn how to deal with everyday life. If the operative result is not satisfactory, another surgical procedure may promise success.
However, this therapy always depends on the specific situation. In addition, those affected can realize some aspects themselves that reduce the complications of constipation and incontinence. Choosing suitable foods can be learned. Colon irrigation on the toilet also relieves symptoms.
You can do that yourself
Surgical treatment is always required for anal athresia. The most important self-help measure is to clarify the complaints quickly and to make an appointment for a surgical procedure as soon as possible. The doctor's instructions must be followed before the procedure. The doctor will recommend an individual diet to the patient, which includes avoiding stimulants and certain foods. Patients who regularly take medication or who have allergies that have not yet been recorded in their medical records should inform their doctor.
Since the hospital stay usually lasts several days, a sick leave is usually necessary. After the procedure, rest and bed rest apply. As lying down can be uncomfortable for the first few days, a special hemorrhoid pillow must be used. To ensure that healing is positive, the wound must be well cared for. Precautions should be taken, especially when defecating. The responsible doctor can best answer which measures are necessary and useful in detail.
In general, a doctor must be consulted at least two to three times after an operation, who will monitor the healing process and adjust the medication if necessary. If there are complaints or complications, medical advice is required.


.jpg)




















