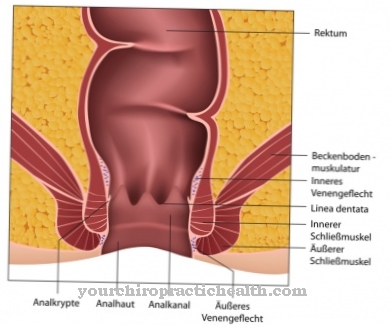
In the Anal fissure or. Anal crack it is a tear in the skin or mucous membrane of the anus that can be very painful. Anal fissures heal poorly due to the location and the physical strain on the affected area of the body and can take a chronic course.
What is an anal fissure?
.jpg)
The term “fissure” comes from the Latin and means “gap”. Accordingly, the anal fissure is a gap-shaped tear in the anal canal skin. This skin at the bottom of the anal canal is very sensitive. If there is a tear, an elongated, crevice-shaped ulcer forms.
An anal tear is usually closely connected to other diseases or complaints in the area of the rectum. These include hemorrhoids, anal cancer, coccyx fistulas and anal abscesses. Since most people find diseases of the anus uncomfortable or embarrassing, they go to the doctor late, which can lead to further complications. A doctor should therefore always be consulted quickly in the event of anal problems.
causes
An anal fissure can have different causes. First of all, an anal fissure can result from hard stool. Chronic constipation promotes hard bowel movements and thus the possibility of an anal fissure.
Persistent diarrhea can also cause the anal skin or mucous membrane to tear. The inflammation leads to permanent irritation of the sensitive anal canal skin.
Furthermore, hemorrhoids are among the favorable factors. Anal fissures can also occur as a result of an underlying disease, such as Crohn's disease.
Longstanding laxative abuse can also be a cause. Various sexual practices, such as anal intercourse, are also possible causes of an anal fissure.
Symptoms, ailments & signs
An anal fissure often causes stabbing or burning pain during bowel movements. Usually the symptoms persist for a few hours after defecation. Externally, an anal fissure can be recognized by the typical tears in the anus.
These usually bleed and cause bright red spots on toilet paper or stools. This can be accompanied by unpleasant itching, burning and oozing in the area of the anus. Many patients also suffer from constipation. If the anus tear is based on hemorrhoids, further symptoms such as pain when sitting and infections at the anus may develop.
An anal fissure can also lead to cramps. This means that you have to press harder when going to the toilet. In the long run, the connective tissue around the muscle can multiply and eventually harden. Such a severe course manifests itself in increasing pain, bleeding and cramps during bowel movements. An anus tear sometimes also results in psychological complaints.
Some people affected develop a fear of going to the toilet, which leads to stool retention and consequent constipation. A mucosal secretion is characteristic of a chronic or recurring anal fissure, which can be determined by means of transparent discharge and increasing bleeding.
Diagnosis & course
The doctor makes the diagnosis based on interviewing the patient and inspecting the anus. Usually the anal fissure is in the six o'clock position ... towards the tailbone. The fissure in the direction of the dam is less common. When palpating, the doctor may feel an ulcer that causes pain to the patient.
An anal fissure manifests itself in the following symptoms: fresh, pale blood, pain when defecating (sharp pain and persistent burning sensation after defecation), spasm of the sphincter, itching.
Due to the reflex spasm of the sphincter, the chair is often only released as a thin stream. Fear of the next bowel movement often leads to constipation. A vicious circle develops: the blockages lead to a tear in the anal skin and pain during bowel movements. For fear of the pain, the stool is held back, there is a spasm of the sphincter, which in the end increases the pain again.
However, all these signs can also indicate other diseases of the intestine and must therefore also be clarified using a differential diagnosis.
An acute anal fissure can heal spontaneously or with appropriate treatment. But it can also recur and even become chronic. It is not uncommon for a connective tissue benign tumor, a so-called anal papilla, to form.
Complications
An anal fissure can be very painful. It should therefore not only be treated immediately with ointments, but also requires special care. The fissure can become inflamed as a complication. The reason lies in the germs that can penetrate the anal fissure during stool passage.
The deep crack in the anus is predestined to be subject to germ contamination. This is especially true with chronic anal fissures. These are to be seen as an open wound. Since stool is excreted one to several times a day, the anal fissure comes into contact with intestinal germs several times a day. One possible complication is fistula formation. The inflammation this causes can spread and affect the surrounding tissue.
Another complication of an anal fissure is the development of an anal abscess. This is an encapsulated, purulent focus of inflammation in the surrounding tissue. This complication leads to significant pain. The area around the anal fissure is hardened and plump. A fever with chills may develop. An anal abscess cannot be repaired without surgical intervention.
To prevent such complications, anal fissures should be avoided whenever possible. Causes such as a low-fiber diet and chronic lack of exercise can be eliminated. Certain sexual practices should be avoided if there is a tendency to fissures. Colon exams and medical check-ups can help prevent complications.
When should you go to the doctor?
As a general rule, treatment of an anal fissure should not be delayed. Sufferers can try for a few days to get relief with hip baths, ointments and a diet that leads to loose stools. However, if the pain, bleeding and other symptoms worsen or remain the same, a specialist must be consulted. Proctologists and gastroenterologists come into question here.
Otherwise, because of the poor wound healing in the anal area, those affected risk the transition to a chronic anal fissure, which is associated with many complications.
If the person develops other symptoms, such as fever, nausea, and body aches, this is an indication of a secondary infection. This can easily occur with a torn mucous membrane. In addition, it can lead to pus formation and inflammation, which cause further pain and itching, which must also be clarified by a doctor.
A doctor should also be consulted in the case of recurring anal fissures. After all, there can be reasons for this in the sphincter muscle and the surrounding tissue itself. This should happen regardless of whether the person concerned can identify possible causes for their anal fissure or not.
Surgery should be considered if conservative therapies for alleviating and healing an anal fissure are unsuccessful.
Doctors & therapists in your area
Treatment & Therapy
In the case of an acute anal fissure, the regulation of the bowel movement is the decisive measure. This includes a diet rich in fiber and a high level of fluid intake. With a healthy diet, the anal canal expands naturally and the stool is permanently soft and shaped.
The doctor prescribes an ointment with a local anesthetic, i.e. an ointment that numbs the skin locally, to prevent the pain and burning sensation during or after bowel movements.
Of course, careful anal hygiene with pH-neutral soaps is also important. Warm chamomile baths can also help. With these measures, an acute anal fissure heals within six to eight weeks.
With a chronic anal fissure, symptoms last for more than two months. In addition to all measures in the treatment of an acute anal fissure, the doctor now also prescribes drugs with the active ingredient nitroglycerin. Calcium antagonists (nifedipine and diltiazem) are also used. These agents relax the sphincter muscle.
The patient must apply the ointments three to four times a day for the next 6-12 weeks. In most cases this also heals a chronic anal fissure.
However, if there is no cure, although the patient consistently adheres to the appropriate diet and also applies the prescribed ointments exactly, the doctor must consider an operation. Here the fissure is removed together with the scarred tissue. However, wound healing takes a long time since the doctor usually does not use a suture.
Outlook & forecast
Smaller anal fissures, especially those caused by injuries, often heal on their own within a few days or weeks if the area in question is kept clean and excessive strain on the anus region (straining when defecating, stool that is too hard, sexual practices in the anal area) is prevented . Smaller fissures heal without any consequential damage.
The extent to which the injured area is spared is decisive for the healing process. Irritation and muscle tension in the corresponding area have a counterproductive effect, while gentle behavior, warm hip baths, etc. have a positive effect.
Bacteria also play a role. If a fissure becomes inflamed, spontaneous healing is no longer to be expected. Ointments, hip baths and other measures are now necessary at the latest.
If an inflamed anal fissure is not treated by a doctor, the prognosis is poor. Subsequent complications are then common and worsen the clinical picture. Irreversible damage can occur for the person affected, as the sensitive tissue of the anus region is pathologically changed by an inflammation.
In addition, a chronic - that is, recurring and not permanently healing - anal fissure can develop if the person concerned spreads inflammation and structural damage in the corresponding area. An operation (e.g. a fissurectomy) may therefore be necessary afterwards.
However, the prognosis for anal fissures is overall good.
prevention
The best prevention against an anal fissure is a healthy, high-fiber, balanced diet, enough exercise, and adequate hydration.
Aftercare
The anal fissure (anal tear) can be treated both conservatively and surgically. It depends on the severity of the condition and the needs of the patient. Depending on which option of therapy is chosen, the follow-up care is also somewhat different.
In many cases, those who opt for conservative treatment can do without follow-up care. Because the anal fissure is clearly noticeable through stabbing pain and bleeding, those affected also notice when the treatment with creams, anal stretchers or stool softening agents has been successful. Only if the impression arises that the symptoms have not completely receded is a visit to the doctor again advisable for follow-up care.
The contact person here is the proctologist or the family doctor who is experienced in this area. If the patient does not feel any discomfort, aftercare often includes the application of ointments and consistent fiber-rich food including a large amount of drinking for aftercare and at the same time prevention of a new crack.
After surgery, follow-up care by the proctologist is important. It controls wound healing, for example with regard to infection. He can also make sure that the stool did not cause a recurrence after the operation. He controls the tone of the muscles of the sphincter and can give tips on how to avoid strong pressure, which is counterproductive for fissure healing.
You can do that yourself
If you suspect an anal fissure, it is always advisable to see a doctor first. In addition, the symptoms can be alleviated by good anal hygiene and gentle care products, among other things. It is also important to have enough exercise, for example in the form of pelvic floor muscle training or yoga. In addition, attention should be paid to a healthy and balanced diet. Foods rich in fiber and plenty of fluids guarantee a pleasant and regular bowel movement and thus contribute to the healing of an anus crack.
If there is already constipation, laxatives are also recommended temporarily. Anesthesia can also be performed if the pain is severe. Even mild pain relievers can be taken in consultation with the doctor to alleviate acute symptoms. If the symptoms worsen despite all measures, special preparations from the pharmacy can be used.
Corresponding ointments and lotions contain active ingredients such as lidocaine and bufexamac, which have an analgesic and anti-inflammatory effect on hemorrhoids. Alternatively, we recommend special suppositories, anal stretchers or hip baths.
Early application is crucial in order to avoid further intensification of the anal fissure. In the case of particularly severe or recurring symptoms, you should always see a doctor with an anus tear.

.jpg)




.jpg)