To a Analgesic nephropathy it comes from years of use of certain pain relievers. In the worst case, chronic interstitial nephritis results in complete kidney failure.
What is analgesic nephropathy?

The analgesic nephropathy is also called in medicine Phenacetin kidney. What is meant is a chronic tubolo-interstitial nephropathy, which is caused by prolonged abuse of various painkillers. The most important component is the active ingredient phenacetin.
In addition, non-steroidal anti-inflammatory drugs such as acetylsalicylic acid (ASA) and paracetamol are also considered possible triggers. The proportion of analgesic nephropathy in terminal kidney failure is between one and three percent. The disease is much more common in women than in men.
Women use pain medication more often than men. People who regularly take phenacetin or mixed analgesics are 20 times more likely to develop analgesic nephropathy than other people. In 1986 phenacetin was banned in Germany. Since then, the disease has almost completely disappeared in the Federal Republic.
causes
In earlier years, the cause of analgesic nephropathy was the constant use of drugs containing the active ingredient phenacetin. These were not infrequently offered as mixed preparations. In addition to phenacetin, they also contained caffeine and codeine. By using mixed preparations with paracetamol there was a two to three times higher risk of developing analgesic nephropathy.
Analgesic nephropathy was particularly widespread in the GDR, Australia, the USA, Switzerland, Belgium, Sweden and Eastern Europe. In West Germany, the proportion of people with analgesic nephropathy was between four and nine percent among patients requiring dialysis.
Despite the continued use of paracetamol mixed analgesics, analgesic nephropathy almost completely disappeared after the ban on phenacetin. Phenacetin and its metabolite paracetamol have the property of inhibiting prostaglandin synthesis. Prostaglandins are tissue hormones that induce pain and inflammation.
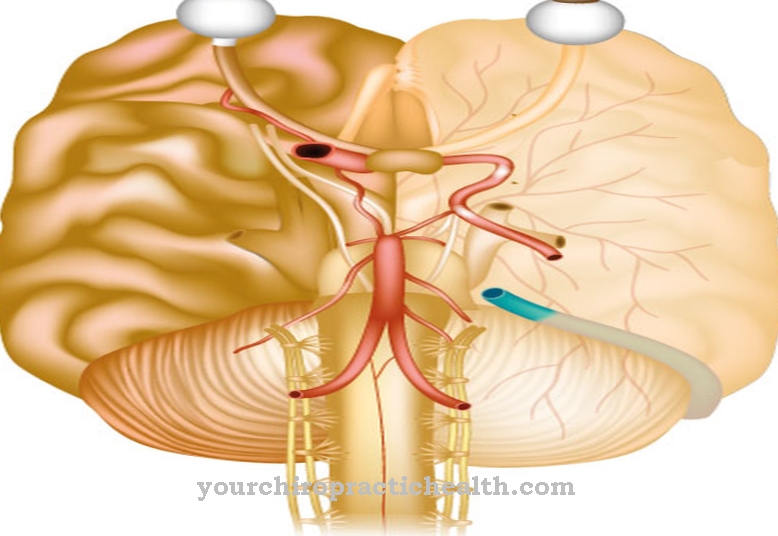
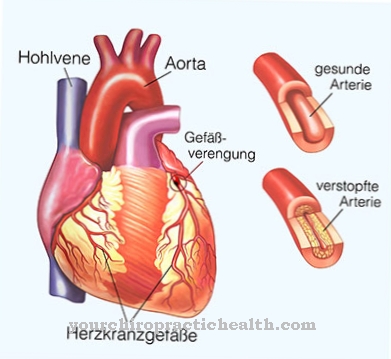
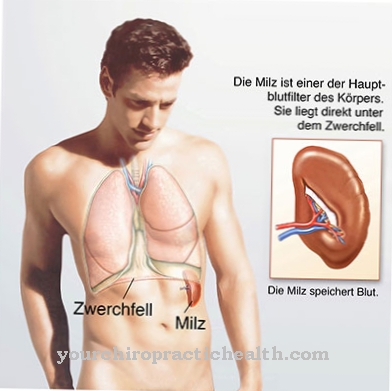
The prostaglandin E2 is inhibited, which is responsible, for example, for an expansion and increased blood flow to the renal medulla. The constant drug-induced inhibition causes the elimination of the vasodilation (vasodilation), which in turn results in a permanent reduced blood flow to the renal medulla. This leads to the development of ischemia and papillary necrosis.
Symptoms, ailments & signs
In the initial stage of analgesic nephropathy, no symptoms can be perceived at first. As the disease progresses, symptoms such as exhaustion and headaches arise. The affected person's skin is brown-gray in color. Furthermore, the signs of anemia (anemia) become noticeable.
They are caused by gastrointestinal bleeding, hemolysis and the formation of sulf and methemoglobin. If necrotic papillae spontaneously come off, there is a risk of ureteric colic. Other signs of analgesic nephropathy include hypokalaemia, hyponatremia, recurrent urinary tract infections, and distal renal tubular acidosis.
Due to a reduced ability to concentrate urine, tubular dysfunctions are also possible. In the worst case, end-stage chronic kidney failure occurs. A possible late complication of misuse of phenacetin is an increased risk of urothelial carcinoma.
Diagnosis & course
If analgesic nephropathy is suspected, the doctor first looks at the patient's medical history in detail. It may be necessary to identify possible abuse of pain medication. A total consumption of more than 1000 grams of phenacetin is considered to be groundbreaking.
If a drug abuse is suspected, the breakdown product N-acetyl-paraminophenol (NAPAP) can be determined in the urine. A daily intake of one gram of phenacetin per day for a period of one to three years was set as the lower limit for the development of analgesic nephropathy. The same applies to a total of one kilogram of phenacetin together with other pain relievers.
The diagnosis of analgesic nephropathy includes various examination methods. These include the 24-hour urine collection, the detection of normochromic anemia, the detection of hematuria, an elimination program and the measurement of blood pressure. As part of an ultrasound examination (sonography) or a computed tomography (CT), reduction in the size of the kidneys, calcifications on the papillae and papillary necrosis can be diagnosed in the advanced stage.
Leukocyturia may be present in the urine sample. The differential diagnosis of other chronic tubolo-interstitial kidney inflammations is also important. The same applies to diabetic nephropathy, sickle cell anemia or urogenital tuberculosis.
If the harmful active substance is discontinued before terminal kidney failure occurs, the analgesic nephropathy usually takes a positive course. In this case, the disease is stopped in time.
Complications
An analgesic nephropathy arises from the abuse of painkillers, which has various complications. In general, analgesics can lead to the development of addiction, the person concerned can become dependent on the painkillers and shows withdrawal symptoms after stopping the drug, which causes both physical and psychological symptoms. Certain analgesics can also acidify the blood. In addition, the risk of ulcers in the gastrointestinal area is increased.
The nephropathy can lead to kidney failure. This leads to a severe impairment of the quality of life. First, there is an increased flow (polyuria), which quickly dries up again (oliguria). In addition, there is an increase in the concentration of urinary substances in the blood such as creatinine, but also toxins such as ammonia. Ammonia can cause blood poisoning (uremia).
In addition, ammonia can pass into the central nervous system and lead to encephalopathy. In the worst cases, dialysis has to be intervened. Furthermore, kidney failure is associated with a reduced excretion of potassium (hyperkalaemia), which can lead to cardiac arrhythmias. Disturbances of the acid-base balance due to a reduced excretion of acids by the kidneys again favor hyperkalemia. In addition, the reduced excretion of fluids increases the risk of edema.
When should you see a doctor?
Analgesic nephropathy should always be examined and treated by a doctor. The doctor should especially be seen if the person concerned has been taking pain medication for a long time. As a rule, the patients suffer from severe headaches, tiredness and fatigue. If the affected person's skin continues to turn brown or gray, a doctor must be consulted.
Immediate treatment is also necessary for symptoms of anemia. Those affected can suffer kidney failure in the further course. If there are problems with the kidneys or the urinary tract, a doctor must be consulted urgently. Bleeding in the stomach and intestines can also be symptoms of analgesic nephropathy and should be investigated. As a rule, the person concerned can initially contact a general practitioner. If the complaints are acute, an emergency doctor can be called.
Doctors & therapists in your area
Treatment & Therapy
An analgesic nephropathy is always in need of treatment. The most important step in therapy is stopping the triggering medication. In addition, it is important to consistently treat the anemia and existing urinary tract infections such as pelvic inflammation. This can include, for example, the administration of antibiotics and switching off the risk factors.
A sufficient supply of fluids is also important. If there is already renal insufficiency, this must also be treated. If there are only slight or moderate functional impairments, further deterioration should be counteracted. These include, among other things, a reduction in table salt and a protein-reduced diet.
In the case of chronic kidney failure, only dialysis (blood washing) or even a kidney transplant can help at an advanced stage. In the latter case, a suitable donor organ is required.
Outlook & forecast
In the worst case, analgesic nephropathy leads to complete kidney failure of the patient. The affected person then usually has to rely on dialysis and a kidney transplant in order to survive.
As the disease progresses, it is not uncommon for infections to occur in the urinary tract, which lead to relatively severe and above all burning pain when urinating. The pain in general can have a negative effect on the psyche of the person concerned and possibly lead to depression or other psychological disorders.
Analgesic nephropathy also leads to bleeding in the stomach and intestines, which leads to relatively severe pain. Those affected suffer from headaches and also from severe exhaustion. The anemia also significantly reduces the resilience of the person affected, so that there are various restrictions in the patient's everyday life.
As a rule, analgesic nephropathy must be treated with the help of drugs to limit various inflammations. Those affected must continue to take it easy and are not allowed to perform strenuous activities. Whether there will be a reduction in life expectancy due to analgesic nephropathy cannot generally be predicted.
prevention
The best preventive measure against analgesic nephropathy is to avoid pain medication abuse.Taking phenacetin is no longer possible nowadays because the drug has been banned since 1986.
Aftercare
Follow-up care should, among other things, prevent the recurrence of an illness. In the case of analgesic nephropathy, this can best be achieved by avoiding the triggering substances. Phenacetin has been banned since 1986. As a result, the disease barely exists in Germany.
Doctors know about the negative consequences and no longer prescribe appropriate preparations. Basically, patients repeatedly suffer from the typical symptoms after ingesting the triggering substances. Immunity does not build up. If therapy is started before renal insufficiency, there is a good prospect of a cure.
Possible complications involve the kidney. This regularly fails if there is no acute treatment and the triggering substances have been in the bloodstream for a long time. Then patients must have regular dialysis. A transplant is usually recommended to improve the quality of life. Scheduled follow-ups include a medical history, urine samples, blood tests, and sonography.
As time goes on, people will need to take medication to prevent inflammation. In everyday life, it is advisable to take a number of preventive measures. These include a high fluid intake, muscle relaxation techniques and at least light physical activity. These and other measures have a pain-relieving effect. A doctor can temporarily order therapy.
You can do that yourself
Patients with analgesic nephropathy can make a significant contribution to improving their disease. This is especially true if the kidney failure was diagnosed in a reversible stage.
First and foremost is behavior change. The use of painkillers should be completely avoided. An alternative treatment for the underlying disease that works without taking painkillers is conceivable. In addition, behaviors can be practiced with which chronic pain can also be controlled without having to take analgesics.
Autogenic training and progressive muscle relaxation can help relieve pain. It is also advisable to integrate exercise and sport into everyday life. This avoids secondary diseases caused by a lack of exercise. Physical activity and sport themselves have a pain-relieving effect due to the release of happiness hormones. Sport in a group with people of similar physical ability is ideal.
In addition, an appropriate diet is important. A high fluid intake helps the kidneys to regenerate. Water, bladder and kidney teas or very diluted juices are suitable drinks. Foods rich in potassium and sodium should be avoided. However, vitamins should be substituted if they cannot be adequately taken in with food. Due to the unfavorable nutrient composition and the high density of salts, the consumption of ready-made meals is not indicated. The therapy also supports a reduction in proteins.

.jpg)

.jpg)


.jpg)