Antihistamines, Histamine receptor antagonists or Histamine receptor blockers, are medicines that are used to treat allergic reactions to neutralize the effects of the body's own histamine. Antihistamines were discovered in 1937 and used therapeutically for the first time in 1942.
What are antihistamines?

Antihistamines are used in the body's allergic immune reactions to neutralize the effects of histamine. Histamines bind to receptors in order to trigger an immune response in the body. Antihistamines block the docking sites of the receptors, of which there are four different types: H1, H2, H3 and H4 receptors.
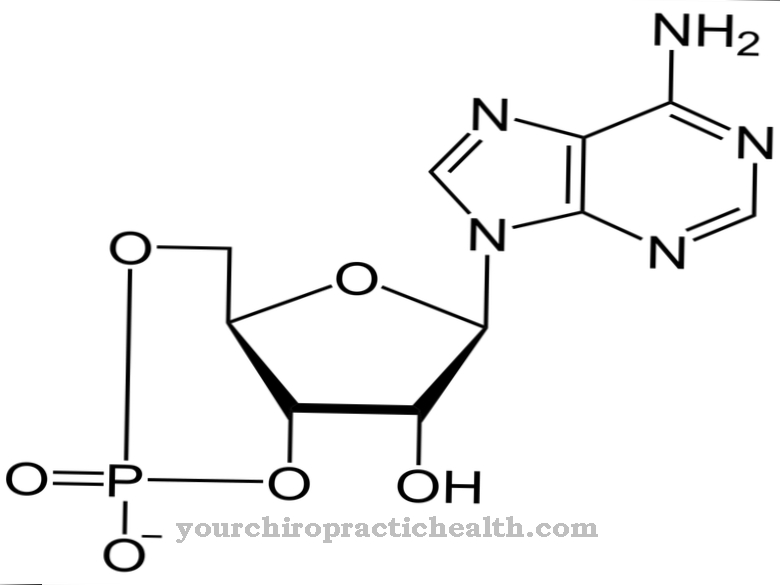
Histamine is a hormone produced by the body and is in an inactive form mainly in the mast cells and leukocytes, which are part of the immune system. If the body is exposed to antigens - substances that are foreign to the body and trigger allergies - these stick to the leukocytes or to the so-called immunoglobulin E, which is located on the surface of the leukocytes.
The leukocytes are destroyed and the histamine stored in them is released. In order to reduce the consequences of the release of histamines and to prevent further release of histamines, antihistamines are prescribed and administered by the doctor.
Application, effect & use
Antihistamines are used for allergic reactions. Antihistamines not only block the receptors so that histamines cannot bind to them again, they also work against the histamine that has already been released by the leukocytes. The receptors are divided into four groups: H1, H2, H3 and H4 receptors.
The H1 receptors cause the following reactions in the body: The blood vessels expand, resulting in a drop in blood pressure. The vessel walls become more permeable. As a result, edema (water retention) occurs in addition to reddening of the skin. As the blood vessels dilate, the H1 receptors in the bronchi produce the opposite effect.
Asthmatics in particular are at risk, as the bronchi can become life-threatening. In addition, the H1 receptors stimulate the transmission of stimuli to the nerves, so that the skin reacts over-sensitive to touch and itching occurs.
If the histamines bind to the H2 receptors, this triggers reactions in the cardiovascular system. The heart rate increases and the pulmonary vessels expand. Furthermore, they have an inflammatory effect on the gastric mucosa and stimulate gastric acid production, which can lead to gastric mucosal inflammation and heartburn.
When histamine binds to H3 receptors, self-regulating processes occur. The release of histamine is inhibited. Research into the H4 receptors is still in its infancy, but it is believed that they have an effect on allergic asthma.
Antihistamines cancel the effects of the hormone histamine. Because of this, there are two types of antihistamines: H1 and H2 antihistamines. H1 antihistamines are mainly used for hay fever, urticaria (hives) and other allergic reactions (watery, itchy eyes, runny nose, shortness of breath, etc.).
H1 antihistamines have a spasmolytic (antispasmodic) and vascular sealing effect. The already dilated blood vessels narrow, the permeability of the vessel walls is reduced, so that edema, reddening of the skin and itching recede. H2 antihistamines block the H2 receptors so that no inflammatory reactions can be caused in the stomach. H2 antihistamines inhibit the production of stomach acid.
Depending on which active ingredient is used, its effect sets i. d. Usually between 30 and 60 minutes. After about three hours the max. Effectiveness usually reaches and lasts for a day, with the effect gradually waning over the course of the hours.
In addition to treating allergic reactions, antihistamines are also used to treat gastric ulcers, ADHD, sleep disorders, and Alzheimer's.
Herbal, Natural & Pharmaceutical Antihistamines
Antihistamines are so far only on the market as H1 and H2 antihistamines and are divided into so-called three generations: antihistamines of the 1st generation, the 2nd generation and the 3rd generation.
1st generation antihistamines include a. the following groups of active ingredients: Bamipin, Clemastin and Dimetinden, Promethazine, Diphenhydramine, Ketotifen and Dimenhydriant. These medicines have many side effects. Because of this, they are no longer used in oral form (tablets, etc.). It is mainly used externally with the help of ointments, drops, gels and creams.
With the development of the 2nd generation antihistamines, the above-mentioned Side effects are reduced or no longer occur. 2nd generation drug groups are u. a. Azelastine, cetirizine, loratadine, levocabastine, fexofenadine, and mizolastine.
The dosage forms are tablets, capsules, sustained release tablets, ointments, nasal sprays, eye drops and, in the case of acute and severe allergic reactions, injection or infusion solutions. Some of the antihistamines are available in pharmacies without a prescription (mainly the 2nd generation), but there are also prescription drugs (1st generation) that must be prescribed by a doctor.
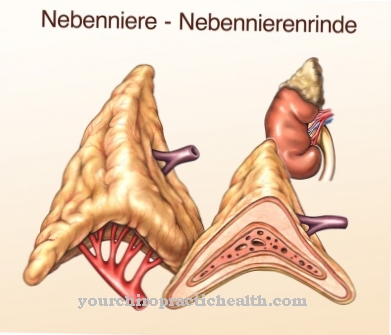
In addition to chemical-pharmacological products, there are also natural antihistamines that, in combination, can reduce the body's allergic reaction. Ascorbic acid, ascorbate and ascorbyl palmitate (vitamin C) ensure that the histamine is broken down more quickly. Pantothenic acid (vitamin B5) is an important building block in the production of cortisol in the adrenal glands. Cortisol has anti-inflammatory properties. Calcium and zinc can block the docking points of the receptors so that the histamine cannot establish itself. Manganese can block the release of histamine and accelerate the breakdown of histamine.
Flavonoids are antioxidants that can have anti-inflammatory effects. The flavonoids hesperidin, rutin and quercetin can have a stabilizing effect on the mast cells so that they cannot be destroyed by the antigens and the histamine cannot be released.
Risks & side effects
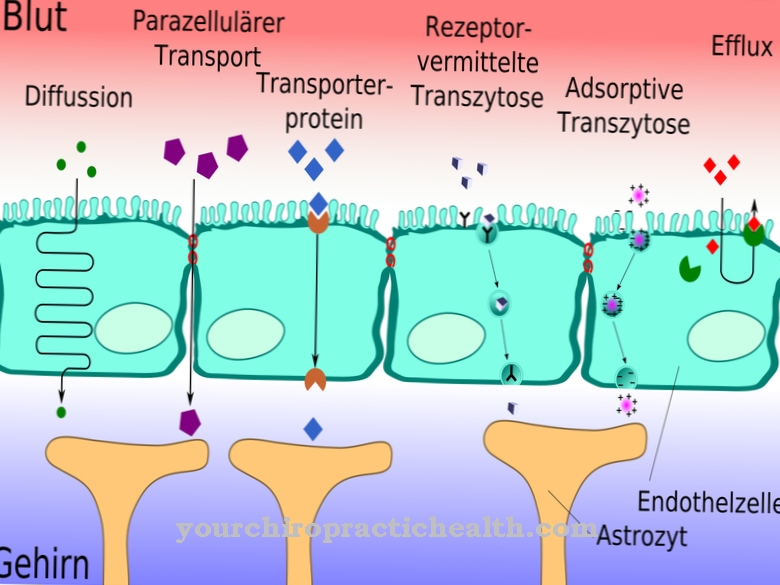
Antihistamines 1st generation have many side effects. H1 antihistamines are easily accessible to the CNS, which means that they can cross the blood-brain barrier so that they work directly in the brain and spinal cord. As a result, side effects such as tiredness, drop in blood pressure, rapid heartbeat, headache, nausea, vomiting and impairment of liver and kidney function can occur.
Since antihistamines of this group have a sedative (drowsy) effect, the ability to drive and use machines is severely restricted. If there are cardiac arrhythmias, glaucoma (glaucoma), epilepsy, asthma and liver and kidney dysfunction, 1st generation H1 antihistamines must not be taken as they favor these diseases. Antihistamines should not be used during pregnancy and breastfeeding.
2nd generation antihistamines can no longer penetrate the blood-brain barrier, so that the side effects are considerably reduced. However, the o.g. Side effects occur, but their occurrence is much less common.
Side effects can also occur with natural antihistamines. An overdose of vitamins and minerals can lead to cardiovascular diseases (including myocardial infarction) as well as kidney and liver dysfunction.
Drug interactions
Antihistamines 1st generation in combination with von tricyclic antidepressants can lead to the formation of glaucoma (glaucoma). Preparations from the active ingredient groups azelastine and cetirizine must not be combined with one another, since cardiovascular diseases can result due to the interactions.
Antihistamines must not be taken together with analgesics (pain relievers), sleeping pills and anesthetics. H1 and H2 antihistamines must not be taken together with beta blockers and ACE inhibitors (medicines for high blood pressure) or with blood coagulants (warfarin).




.jpg)











.jpg)