The Temporal arteritis is an inflammatory disease that primarily affects the elderly. Early therapy usually leads to rapid symptom relief.
What is temporal arteritis?

© blueringmedia - stock.adobe.com
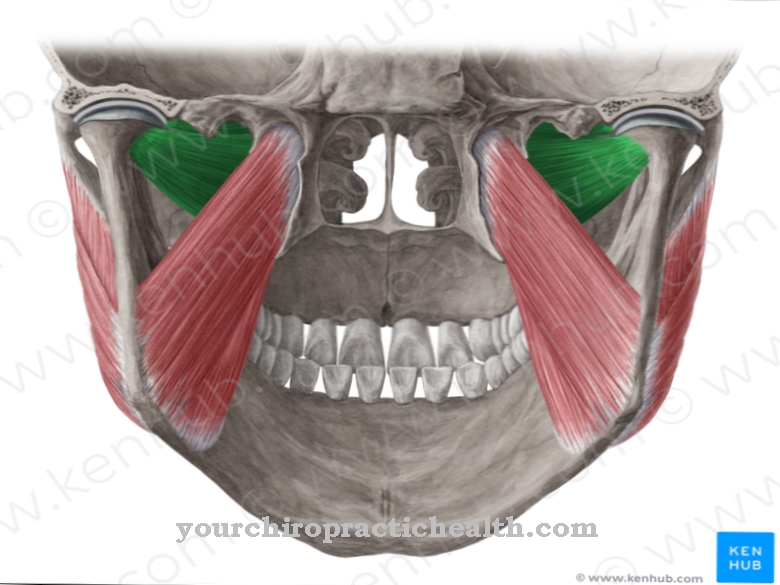
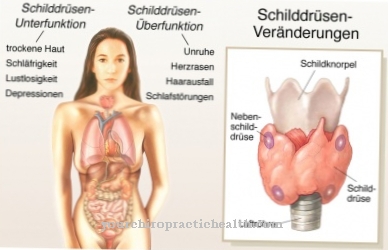
Temporal arteritis is an inflammatory autoimmune disease (a disease in which the body's own immune system falsely turns against the body's own tissue) that primarily affects the temporal arteries (arteries temporales).
Alternative terms for temporal arteritis are, for example Horton's disease or Giant cell arteritis. Temporal arteritis almost exclusively affects people over the age of 50. Temporal arteritis is around three times as likely to affect women as men.
The first symptoms of temporal arteritis include, in a large number of patients, particularly pronounced, sharp headaches. This headache usually intensifies while chewing. In a smaller percentage of those affected, temporal arteritis is a sudden loss of vision in one eye.
Occasionally, the autoimmune disease can also be accompanied by symptoms such as paralysis of the eye muscles as well as fever, muscle pain and fatigue.
causes
The causes of temporal arteritis have not yet been conclusively clarified in medicine. A genetic component of temporal arteritis is assumed - if the disease occurred, for example, in the parents and / or grandparents, there is an increased risk of developing temporal arteritis yourself.
A possible influence of infectious diseases on the occurrence of temporal arteritis is also discussed: It is possible that various viruses and bacteria are able to provoke the development of temporal arteritis.
Corresponding viruses include mainly influenza or flu viruses and the hepatitis B virus. The bacteria that can possibly promote the occurrence of temporal arteritis are primarily the so-called Borrelia - a helical type of bacteria.
You can find your medication here
➔ Medicines for headaches and migrainesSymptoms, ailments & signs
As a rule, the complaints and symptoms of temporal arteritis are relatively clear and point directly to the disease. For this reason, the disease can be diagnosed and treated relatively early on. Those affected suffer primarily from a severe headache. This occurs mainly in the area of the temples and has a very negative effect on the quality of life of the person affected.
It can also cause headaches when chewing or speaking. Temporal arteritis also leads to severe visual disturbances, so that those affected suffer from blurred vision or double vision. Generally speaking, it also decreases eyesight. Those affected also suffer from permanent tiredness and fatigue, which usually cannot be compensated by sleep.
Sweats are common at night and patients continue to experience severe weight loss from temporal arteritis. The symptoms do not always have to occur together, so that a doctor should always be consulted if some complaints persist. With temporal arteritis, the headache can also spread to the ears or eyes.
Diagnosis & course
Temporal arteritis can be diagnosed, for example, on the basis of the so-called ACR (American College of Rheumatology) criteria. These criteria describe, among other things, typical symptoms of the autoimmune disease.
If an affected person meets a certain number of criteria, it can be assumed (with initially limited certainty) that temporal arteritis is present. The diagnosis can be confirmed, for example, by removing tissue from the temporal artery, by ophthalmological examinations or by blood tests. Ultrasound images can also provide further diagnostic information about the presence of temporal arteritis.
With proper therapy, the symptoms of temporal arteritis often subside completely within approx. 6 - 24 months. However, medicine does not speak of a cure in the narrower sense, because in some cases relapses of the disease are possible. In individual cases temporal arteritis can take a chronic (long-term) course.
Complications
If the branches of the carotid artery are affected by temporal arteritis, medical countermeasures must be initiated. The diagnosis, also known as Horton's disease, causes numerous complications, especially when the temporal artery is affected. If the patient concerned receives insufficient or no medical help, the optic nerve is permanently damaged.
There is a risk of blindness and a stroke. As soon as the inflamed aorta narrows, important nerves and supply areas are no longer supplied with blood. Exhaustion, stabbing headaches, aneurysms, weakness of the eye muscles, visual disturbances and attacks of fever can cause permanent discomfort if the disease is not recognized in time.
The special risk group for temporal arteritis includes people from mid-life, the majority of whom are women. The disease itself causes various complications, as does the medication. Not all patients tolerate the oral corticosteroids that control the symptom.
These must be taken for a period of one to two years. Consistent medical supervision is observed. Corticosteroids can negatively affect metabolic functions and bone structure. The subsequent symptoms can weaken the immune system, glaucoma or cataracts and osteoporosis, or increase blood sugar levels or weight. On the other hand, the treatment with cortisone is very successful for the body, but it reduces the risk of heart attacks and prevents blindness.
When should you go to the doctor?
Unfortunately, the symptoms of temporal arteritis are not particularly characteristic, so the symptoms can also be confused with another disease. For this reason, people should always seek medical advice if symptoms occur together for no particular reason. In the case of persistent headaches and an inexplicable loss of weight, the patient must definitely consult a doctor.
The pain can occur in the region of the temples and in most cases is not aggravated by speaking or chewing. An advice should also be sought if there is sudden visual disturbance due to temporal arteritis or if the existing visual problems are exacerbated. Most of those affected also suffer from permanent fatigue and fatigue due to temporal arteritis.
The tiredness can usually not be compensated with the help of sleep. Early treatment can alleviate the symptoms in most cases, and the risk of a stroke is also significantly reduced during treatment. First and foremost, the diagnosis is usually made by a general practitioner. The other complaints are finally treated by a specialist, whereby a visit to the ophthalmologist is usually necessary.
Doctors & therapists in your area
Treatment & Therapy
Acute temporal arteritis is usually considered a medical emergency. If there is a suspicion of temporal arteritis, doctors usually administer high doses of cortisone to combat inflammatory processes.
This treatment step, which takes place as quickly as possible, also pursues the purpose of preventing the inflammation from spreading to the vessels of the brain and thus reducing the risk of a stroke that may result. The individually administered cortisone dose in the case of temporal arteritis is based, for example, on guidelines drawn up by the German Society for Neurology; thereafter, a comparatively high dose makes sense, for example, when the patient concerned is threatened with blindness due to temporal arteritis.
A comparatively lower dose of cortisone is recommended for acute unilateral blindness, while the lowest recommendation is made for patients in whom the eye is not affected by symptoms of temporal arteritis. An acute cortisone therapy carried out in this way is usually followed by further cortisone treatment at a lower dose over several months or years.
Outlook & forecast
Temporal arteritis has a good prognosis in healthy people with a stable immune system. Once the condition is diagnosed and treated, symptoms relieve within a few days. Once the inflammation has healed, the patient can also be discharged from treatment as symptom-free. In most cases, however, the healing process takes several months or years. On average, it takes 6-24 months until the consequences of temporal arteritis are healed and the body's own defense system is stable.
The disease occurs more and more in older people. This increases the likelihood of other medical conditions being present. In these cases, the immune system is additionally weakened and the organism has hardly any possibilities to successfully counter the inflammatory process of temporal arteritis. As a result, healing is delayed, which also affects the diseases that are already present.
Acute temporal arteritis threatens the patient's sudden death. The progress of the inflammation cannot be stopped, bleeding occurs and the patient dies of heart failure or a stroke. People who do not receive medical care also live at a greatly increased risk of death. Blindness or dysfunction can occur.
You can find your medication here
➔ Medicines for headaches and migrainesprevention
Since temporal arteritis is presumably genetically favored, the disease can only be prevented to a limited extent. If the assumption is taken into account that viral and / or bacterial infections can promote temporal arteritis, a strengthening of the body's immune system may help to reduce the risk of an autoimmune disease.
Aftercare
Follow-up care aims to prevent the recurrence of temporal arteritis through scheduled examinations. In view of the positive prognosis, no further complaints are to be expected after medical supervision. The regeneration process is sometimes delayed in older people. Immunity does not build up. A chronic form of the disease rarely develops.
The cause of temporal arteritis has not been conclusively clarified. Some scientists assume genetic conditions are the trigger. These cannot be influenced. It is recognized, however, that a strengthening of the immune system prevents a new disease. This is the responsibility of the patient and can be medically verified, for example, through blood tests.
Those affected should make sure they eat a diet rich in vitamins and fiber. Regular exercise is important. Pollutants such as nicotine and alcohol should be avoided. Once ill, they should ensure they get enough sleep and rest. Stress at work and in everyday life should be avoided as far as possible. Temporal arteritis is determined using the criteria of the American College of Rheumatology.
Blood tests and Doppler sonography play a role in this. These can be repeated at regular intervals to avoid further complications. The decisive factor here is avoiding permanent training.
You can do that yourself
Since temporal arteritis can easily be confused with other diseases due to its symptoms, it is often difficult for a layperson to recognize in everyday life. This severely limits the measures and possibilities for self-help.
Since it is an autoimmune disease, the person affected can in principle pay attention to the strengthening of his immune system even without suspecting this diagnosis. With a healthy lifestyle he strengthens his immune system and thus stabilizes his organism. At the same time, the healing process is shortened when there is a strong immune system. A balanced diet rich in vitamins is important for this.
The body needs sufficient nutrients, trace elements and regular exercise. This stimulates the metabolism and prevents fat accumulation. The dead weight should be within the normal weight. At the same time, the body must be supplied with a sufficient amount of fluid every day. Pollutants such as nicotine or alcohol are to be avoided. Sufficient sleep, regular rest and recovery phases are also important to strengthen the organism.
In stressful situations or phases of life, relaxation techniques or communication within a good social environment help to establish inner balance. As soon as the person concerned feels an unexplained discomfort, he should see a doctor and ask for further examinations.

.jpg)
.jpg)

.jpg)
.jpg)