A arthrosis or Joint wear is a disease of the joints. In doing so, irreversible joint damage occurs primarily through persistent incorrect loading. Osteoarthritis can also occur due to cartilage defects and injuries.
What is osteoarthritis?

Arthrosis refers to the increasing damage to the cartilage or the loss of cartilage mass in the joint. Colloquially, it is also known as joint wear. Osteoarthritis is considered to be the most common joint disease in the world. It can basically occur in all joints. Osteoarthritis of the knees or knee joints is particularly common.
Almost everyone is affected by osteoarthritis in the course of their life; one more, the other less strong. Around every 10th to 20th German citizen suffers from osteoarthritis between the ages of 50 and 60, with excess weight causing joint wear. Osteoarthritis is therefore also referred to as the progressive, age-dependent joint disease.
causes
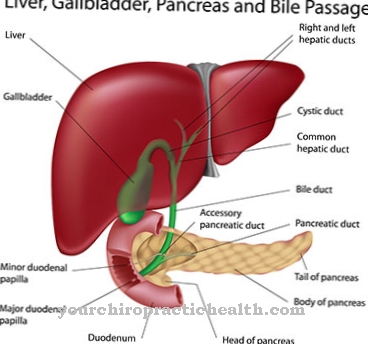
There are many causes of osteoarthritis. In any case, however, the disease is related to stress on the joints. The joint disease can be triggered by acidosis or a lack of exercise. Missing minerals are characteristic. The so-called base deficiency leads to a thickening of the synovial fluid. Uric acid crystals are deposited in the synovial fluid. These lead to an emery-like effect, which causes severe pain.
In addition, the cartilage in the joints is broken down. In principle, one can say that the less cartilage, the greater the pain. Due to the pain, osteoarthritis sufferers avoid any kind of movement. However, due to the lack of exercise, the cartilage is no longer supplied with sufficient nutrients. This speeds up the course of the disease. Since osteoarthritis is always characterized by acidification of the body, a diet with excess acid foods drives the disease forward.
Symptoms, ailments & signs
Typical signs of osteoarthritis are joint pain, stiffness and a loss of mobility in the joints. In the early stages, these signs often do not appear or are only very mild. However, as the disease progresses, these symptoms steadily worsen, and other complaints also arise.
For example, it is characteristic of stress pain that only occurs when the affected joint is stressed. If the walking apparatus is affected, so-called starting pain can also be seen. This refers to pain that occurs after sitting or lying down for a long time, as soon as the patient tries to walk or run.
If the disease is left untreated or if the patient does not respond to therapy, symptoms will continue to worsen. The patient then often suffers from pain in the affected joints even at rest. Inflammation usually occurs, which also affects the synovial membrane and joint capsules.
The doctor then speaks of synovitis. This very often leads to swelling of the joints, so that their size can increase considerably. If the ankles are affected, the patient's shoes often no longer fit. In the case of arthrosis of the finger joints, hard swellings occur again and again, which severely restrict the use of the hands. Some patients also complain of a significant loss of strength, which further reduces motor skills.
course
One symptom of osteoarthritis is pain. However, this usually only becomes noticeable when the disease has progressed. In the early stages, there is initially a small amount of cartilage damage, which is associated with compression of the bone. Bone areas that lie directly under the diseased cartilage show changes.
Over the years, the articular cartilage rubs off more and more until it has finally disappeared completely. If this is the case, two bones rub against each other, causing enormous pain. The friction in the joint increases significantly. A shock absorber is no longer available. Changes in the shape of the joint shorten the ligaments over the years, which leads to instability of the joint.
Complications
A common complication is inflammation of the joint. Joint swelling and pain increase. In addition, fluid can form in the joint. The joint structure can also change fundamentally, i.e. degenerative changes can occur. Bulges and deformations and changes in the ligamentous apparatus can occur.
The bone can thicken under the layer of cartilage. This can lead to a misalignment of the axes, changes in the sequence of movements and greater pain. If the bare bones rub against each other, the surface can collapse locally. Debris gets into the bones, which is later decomposed. A cavity is created.
If not properly treated, osteoarthritis can become chronic. This often severely affects the quality of life. It can lead to insomnia. So stiffness and restricted mobility can hinder a comfortable sleeping position.
Stiff joints with limited range of motion can reduce the desire to exercise. Walking can also be affected. Sedentary lifestyle can lead to other complications, such as weight gain.
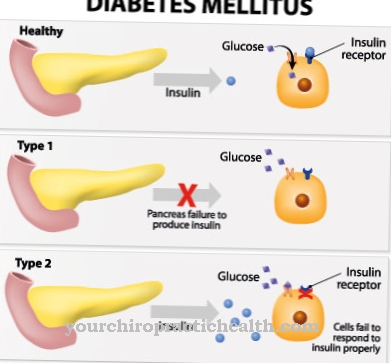
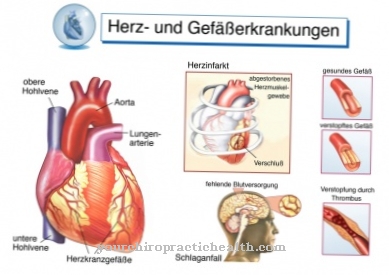
This can worsen osteoarthritis symptoms and cause other complications, such as high blood pressure, heart problems, and an increased risk of diabetes.
People with osteoarthritis are often less productive. They can be absent in the workplace and impaired in their everyday life.
When should you go to the doctor?
As soon as the pain is permanent and restricts mobility, it is advisable to go to a specialist. The rheumatologist uses blood tests and imaging tests to determine how far the disease has progressed. He prescribes pain relievers and anti-inflammatory drugs.
Arthrosis in the fingers, which only causes short-term pain when overloaded, can often be remedied by immobilization. Regular exercise should not be excluded. However, this can be done without stressing the joints. The same applies to osteoarthritis in the knees.
As soon as redness and swelling appear on the affected parts of the body, only a doctor can help. Long-term self-treatment with pain relievers is not recommended. The risk of damage to the stomach is too great. Interactions with other drugs can only be determined by a specialist.
If knots have formed in the joints of the fingers, they do not need to be treated if they are pain-free. If they grow and block nerve pathways, they should be shown to a specialist. This also applies if they are permanently reddened as a sign of inflammation.
Doctors & therapists in your area
Treatment & Therapy
The problem is that osteoarthritis cannot be prevented. There is also no therapy that can eliminate osteoarthritis. However, their development can be slowed down and further deterioration avoided. Physiotherapy, orthopedic aids, medication, operations and subsequent rehabilitation are available as part of therapy.
Any overload of the affected joint should be avoided, for example. Body weight plays a decisive role in this. Obesity should therefore be reduced. Medicines or physiotherapy can relieve the pain and thereby reduce the restriction of mobility. However, since osteoarthritis is a so-called degenerative change in the articular cartilage, a cure is not yet possible. It is also important that the more muscles and ligaments are developed, the more the joint is relieved. Exercise is therefore recommended. Everything is good that is easy on the joints.
This includes cycling, swimming and gymnastics. Exercise promotes blood circulation in the joint and the transport of nutrients to the joint. The muscles are strengthened, joint stability and joint cushioning are improved. In the case of severe pain during movement, those affected should protect their joints with bandages or splints. If the conservative therapies are unsuccessful and the symptoms can no longer be contained, only an operation will help. These include cartilage transplants or artificial joints, which are intended to help ensure that "normal" movement is possible again.
Outlook & forecast
There is no cure for osteoarthritis, but certain sports can prevent the disease from progressing. Above all, sports should be selected in which the stress on the joints is even. These include, for example, swimming or cycling.
It is also important to lose weight in overweight people in order to avoid unnecessary stress on the bones. Orthopedic aids such as insoles or buffer heels also help to compensate for misalignments. Special muscle building training, which makes the patient's movements safer, also has a positive effect.
In principle, a prognosis depends on the individual course. As the joint damage progresses, the symptoms also increase, so it is important to treat osteoarthritis early as well. This can relieve the pain and improve the quality of life. If the disease progresses very slowly, many patients are often pain-free for several months, but if the disease progresses rapidly, an artificial joint replacement may be necessary within a very short time.
With the help of therapeutic measures, attempts are made to prevent the progression of osteoarthritis, whereby there are many methods to choose from, which those affected should also exhaust in order to improve performance.
Aftercare
Osteoarthritis is a joint disease that is usually characterized by progressive wear and tear. Follow-up care after medical treatment in this context means above all that the course is stopped or delayed as best as possible. The active cooperation of the patient is important here in order to optimally organize regeneration and aftercare.
Arthrosis in the joints and spine can be specifically influenced by movement. The joint lubricant (synovial fluid) is increasingly formed through movement and, as a buffer, can significantly reduce the rubbing of joint surfaces as a cause of osteoarthritis. That is why exercise is part of every follow-up care. Strength training and moderate endurance training are recommended here.
Water aerobics and water aerobics are also recommended, as the buoyancy of the water relieves the joints during movement. Learning to behave in a way that is gentle on the back is also part of the aftercare. There are back school courses that are offered in adult education centers, by health insurance companies or physiotherapists. Drinking enough water is also important for joint function. In addition, mobility can be improved through spinal gymnastics or rehabilitation sports.
Muscular imbalances are to be compensated by targeted muscle training. It strengthens weak muscles and stretches shortened muscles so that the joints and spine are held and protected in their physiological position. Sports activity in life is therefore one of the most important behavioral measures in aftercare for osteoarthritis and is best integrated into the daily routine
You can do that yourself
In terms of prevention, it is fundamentally important to pay attention to your own body weight. Every kilogram too much represents a further burden, especially for the knee joint. In addition, as a result of being overweight, negative changes in the metabolism may occur. A balanced and calorie-conscious diet therefore plays a substantial part in preventing the development of osteoarthritis.
Avoiding meat or animal fats in general can help to avoid inflammation. It is also advisable to avoid heavily processed foods, i.e. finished products and fast food. Instead, the diet should ideally consist of plenty of fresh fruit and vegetables, as well as grain products, rice, fish, but also low-fat dairy products.
A high degree of movement is one of the elementary measures to prevent the development of osteoarthritis. The synovial fluid and the nutrients it contains are massaged into the existing cartilage mass through movement. Joint-friendly sports such as swimming, cycling or hiking in flat terrain are particularly suitable. Physiotherapy and physiotherapeutic measures are also advisable. Movements that put stress on the joints should be avoided as much as possible, as well as excessive strain.
In addition, smoking should be avoided, as the consumption of cigarettes can lead to arthritic changes in the joints, which causes a breakdown of the articular cartilage.








.jpg)



.jpg)










.jpg)
