A Asphyxia neonatorum ("Pulselessness of the newborn") is a lack of oxygen in the newborn. Be used as synonyms peripartum asphyxia, Neonatal asphyxia or Childbirth asphyxia used. The lack of oxygen leads to breathing disorders and thus to a breakdown of the circulatory system.
What is asphyxia neonatorum?
The newborn reacts to a poor oxygen supply with respiratory depression. The blood carries too much carbon dioxide with it which cannot be breathed out and which accumulates in the blood and in the organs. When there is a lack of oxygen, the metabolism switches to harmful anaerobic combustion. The pH value of the umbilical cord blood is acidic (acidosis from pH value less than 7.1 or 7.0).
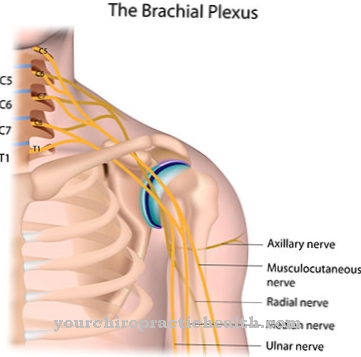
Further consequences of this can be more or less severe damage to different organs; but also malfunctions of the central and peripheral nervous system. About 20 percent of all newborn deaths go to the Asphyxia neonatorum back. Premature babies are 20 times more likely to develop asphyxia.
The risk increases the more factors can be combined and the more serious a single factor is. These include: Birth before the 32nd week of pregnancy, too small and too easy for the pregnancy week. In the case of twin or multiple pregnancies, the risk of asphyxia for the second-born twin is increased - and accordingly for the subsequent children - if the birth is delayed.
causes
Oxygen deficiency can occur during pregnancy, during childbirth and shortly after the birth. As a result of a restricted function of the mother cake or a wrapping with the umbilical cord, the umbilical vein of the unborn child is undersupplied with oxygen and thus the entire organism is insufficiently supplied with oxygen.
This can result in consequential damage. The unborn child has less weight and size gain and starts giving birth with unfavorable conditions. Before birth, both mother and child can go through an infection (example: toxoplasmosis).
The use of medication, drugs, alcohol and nicotine also increases the risk of asphyxia. During embryogenesis, undesirable developments in the genetically designed blueprint may have occurred: The baby starts birth with poor conditions. A sugar disease in the mother also poses a risk for newborn asphyxia.
A very difficult birth can result in massive stress for the baby, so that it turns blue and comes into the world with gasping. Due to their general immaturity, including of the lungs, premature babies have an increased risk of postnatal asphyxia. Cerebral haemorrhage caused by asphyxia can lead to further asphyxia and an adjustment disorder of breathing and organs.
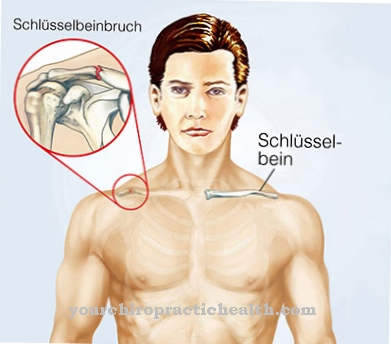
After the birth, the risk of asphyxia is due to immature lungs, lung infections, pathogens in the blood or congenital heart defects. Birth injuries can lead to asphyxia.
Symptoms, ailments & signs
The Apgar value is determined one, five, ten and sixty minutes after birth to describe the adaptation of the newborn from life in the womb to life outside with its own breathing and metabolism. The newborn is born blue and gasped (Asphyxia livida), the Apgar values one minute after birth (4-7) are correspondingly low.
The newborn has an even worse prognosis if it is born as a "white apparent death" (Asphyxia pallida). The Apgar values are almost zero (0-3) one minute after birth. With circulatory weakness, there is weak superficial breathing. An insufficient amount of breathing gases (carbon dioxide and oxygen) is exchanged.
The blood cells in the arteries do not carry enough oxygen in the arteries to supply the tissues: The oxygen partial pressure decreases - not only in the arteries, but in the entire tissue, which turns blue (cyanosis of the skin and mucous membranes). The carbon dioxide that is not exhaled leads to a clouding of consciousness that can even lead to a coma.
The heart rate drops below 100 or below 80 beats per minute. The muscle tone becomes slack. Instead of the expected strong screaming, grimacing or no screaming takes place.
Diagnosis & course of disease
Asphyxia neonatorum is a medical emergency that is met with extensive commitment to ensure that breathing, metabolism and organ function are adapted to life outside the womb. This phase can last a few days or several weeks.
Whether, at what point and to what extent damage to the central and peripheral nervous system, the vegetative nervous system and the organ functions are caused is not completely predictable and varies from case to case. The damage can be assigned to infantile cerebral palsy (ICP).
Treatment & Therapy
In the course of genetic development in early childhood, it becomes clear whether there are developmental disorders or developmental delays. The sucking and swallowing reflex is of central importance for digestion: utilization of nutrients, growth and weight gain.
The innate reflexes are gradually replaced by voluntary movements. The infant should complete the milestones within the timeframe. The baby's and toddler's perception can be observed and is becoming more and more differentiated, as is their language and motor skills.
The pediatrician is trained to determine developmental delays within the U-examinations and to initiate physiotherapy, occupational therapy or early intervention measures as required. Deficits show up in the form of screaming, failure to thrive, underweight. Even in the first few months, the small infant does not carry out certain genetically created movement patterns in the intended way.
If he has a stiff, stretched trunk with overstretched head and legs, this suggests a movement disorder that inevitably leads to motor deficits. Motor deficits are particularly noticeable. They range from spasticity and diparesis of the legs to tetraparesis with increasing need for care. The orthopedic aids range from insoles to orthoses and walkers to wheelchairs.
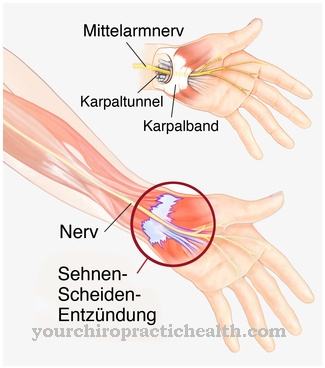
Serious spasticity is attempted to be controlled with antispasmodic agents. If tendons, ligaments and joints or contractures are misaligned, operations are called for, depending on the severity. These can appear on the hips, knees, ankles, feet, toes, shoulders, elbows, and wrists. The more severe the course, the more newborn reflexes remain and the fewer voluntary movements are possible.
If the facial area is affected, there is increased salivation, unclear speech, misaligned teeth and deformation of the palate and problems with chewing and swallowing. Furthermore, there are problems with the ventilation of the nose, ears, and bronchi, so that increased infections are the result.
Due to a lack of erection against gravity and insufficient muscle build-up due to insufficient supply of nutrients (in the trunk as in the entire body), bronchitis and asthma occur more frequently, additionally supported by faulty control of the autonomic nervous system. Sensitivity disorders of the fingertips can exist. Hearing loss can occur.
As a result of incorrect control, a high degree of ametropia is common, usually myopia. Myopia brings with it an increased risk of retinal detachment, retinal degeneration as twilight visual impairment and myopic macular degeneration. For premature babies, there is also the risk of premature retinopathy. In the middle segment of the eye there is a risk of premature cataracts and glaucoma.
Few examples are documented in the literature, according to which the retina can behave in ICP as in retinitis pigmentosa. Optic atrophy can also occur. Retinal detachment and retinopathy of premature infants are treated with laser, cryocoagulation, plomb, cerclage or pars-plana vitrectomy, depending on the severity. The cataract is removed and the eye is fitted with an artificial lens.
There is no therapy for dry macular degeneration, there are various methods to choose from for wet macular degeneration - "Syringe in the eye". The optic atrophy can continue ascending from the ganglion cells to the visual cortex. Retinitis pigmentosa and optic atrophy currently have no therapeutic options. In the end, there is blindness here.
prevention
Pregnant women should carefully observe themselves and their pregnancy, eat healthily and avoid all risks for themselves and the unborn child. These include medication, smoking, alcohol, drugs. She should attend the check-up appointments with her gynecologist. Should she feel that “something is wrong”, she should investigate this feeling and have the cause clarified.
Some structural defects in embryogenesis trigger premature births. Sometimes there are also infections such as toxoplasmosis or candida fungus. If the woman belongs to the group of pregnant women at risk, she should go to a well-equipped clinic. In the delivery room itself, it is to be hoped that the care provided by midwives, nurses and doctors is good, so that if complications arise during the birth, a caesarean section or forceps delivery can be performed, depending on the stage of delivery.
















.jpg)

