As bacterial vaginosis is the name given to the most widespread microbially caused vaginal infection in reproductive women, the cause of which is attributed to an atypical colonization of the female genital area by anaerobic bacteria, mainly Gardnerella vaginalis, and which can be treated well with drugs.
What is bacterial vaginosis?

© designua - stock.adobe.com
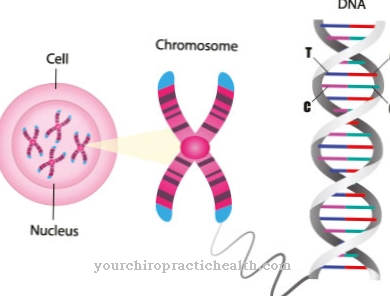
In bacterial vaginosis, a bacterial infection is a disruption of the physiological balance of the vaginal environment.
The healthy vaginal flora, which predominantly contains lactic acid-producing lactobacilli, is slightly acidic with a pH value of 3.8 to 4.5.In bacterial vaginosis, the bacterial balance shifts due to a decrease in the number of lactobacilli, so that the pH value is in the less acidic range and the vaginal flora can be colonized by other bacteria.
One of these is the type of bacteria Gardnerella vaginalis, which often penetrates the vagina at the same time as other anaerobic bacteria, multiplies and leads to a mixed infection. This causes the fishy-smelling vaginal discharge characteristic of bacterial vaginosis, which is one of the core symptoms of bacterial vaginosis and is caused by amines (amine odor).
causes
The imbalance of the vaginal environment that is characteristic of bacterial vaginosis can be caused by several factors. While sexual intercourse increases the risk of infection and is suspected to be the main cause of bacterial vaginosis, psychosocial stress or excessive vaginal hygiene can disrupt the pH value of the vaginal flora and thus promote the colonization of pathogenic germs.
In addition, prolonged menstruation is a risk factor, as the number of estrogen-dependent lactobacilli decreases due to the lower estrogen level during menstruation, which makes the pH less acidic. A less acidic pH value of the vaginal flora can lead to colonization and reproduction of other bacteria and thus trigger bacterial vaginosis.
Symptoms, ailments & signs
Bacterial vaginosis remains asymptomatic in many women. Possible symptoms include redness in the genital area and increased vaginal discharge. The discharge is usually gray-white and thin or sticky, but it can also be bloody or slimy.
In individual cases there are small bubbles in the discharge. The smell of the discharge is usually slightly sour or the discharge smells like fish. Upon contact with semen, the odor increases in intensity. Furthermore, bacterial vaginosis can cause itching in the area of the vagina and labia. Sensory disturbances and abnormal sensations in the external genitalia can also occur.
Affected women feel the vagina is dry despite the discharge or feel an indefinable feeling of pressure on the lower labia. This is often accompanied by pain when urinating and during sexual intercourse. There may also be puffs of air from the vagina, which those affected usually find very uncomfortable.
Additional symptoms can occur as bacterial vaginosis progresses and causes other diseases. This can lead to severe pain that can radiate into the abdomen. Urinary retention and heavy bleeding can also occur, which usually occur outside of your period.
Diagnosis & course
To diagnose bacterial vaginosis, at least three out of four tests on the vaginal swab taken must be positive. A gray-white discharge must be detectable, the fish-like smell of which is reinforced by the so-called amine test (addition of 10 percent potassium hydroxide).
In addition, a pH value of over 4.5 and / or a minimum of 20 percent bacterial colonization of the vaginal cells must be determined microscopically. For a reliable diagnosis of bacterial vaginosis, any other infections (Trichomonas vaginalis, mycoplasma) as well as vaginitis and cervicitis should be excluded.
In the case of bacterial vaginosis, itching and reddening of the skin in the genital area can be observed in rare cases in addition to the gray-white discharge. Bacterial vaginosis can also cause pain during urination and sexual intercourse. Without drug therapy, vaginal vaginosis has a minimal risk of bacterial spread to the upper genital area, which can cause further complications.
Complications
In non-pregnant women, bacterial vaginosis increases the risk of gynecological inflammation. The lining of the cervix can become inflamed (cervicitis). Inflammation of the lining of the uterus (endometritis) and inflammation of the fallopian tubes (salpingitis) can also occur. In addition, the external female genital area and the vaginal entrance (vulvitis) can become inflamed. Inflammation of the Bartholin glands (Bartholinitis) cannot be excluded.
Some complications associated with bacterial vaginosis can also occur in pregnant women. Pregnant women with bacterial vaginosis are at increased risk of preterm labor. They can also suffer premature delivery or premature amniotic sac rupture.
During pregnancy, an infection of the embryonic envelope known as amnionitis can occur. Various complications associated with bacterial vaginosis can also occur after delivery. Inflammation can occur and the healing process of the perineal incision can be delayed. An abdominal wall abscess can occur after a caesarean section. Inflammation of the lining of the uterus is also possible.
Bacterial vaginosis can also be transmitted to men during sexual intercourse. In this context it can lead to a mostly mild and short-lasting inflammation of the glans (balanoposthitis).
When should you go to the doctor?
In most cases the body can regulate an imbalance in the vaginal environment on its own. If you have a healthy lifestyle and a strengthened immune system, a doctor's visit is not absolutely necessary. Women who are in poor health should discuss the symptoms of bacterial vaginosis (e.g. itching, redness and pain when urinating) with their gynecologist as soon as possible. If the course is severe, in which the symptoms increase rapidly and physical and mental well-being deteriorates, a doctor must be consulted immediately.
You should go to the hospital with severe symptoms such as rashes and sharp pain when urinating. This is especially true if the infection occurs during pregnancy. In the worst case, improper or late treatment can lead to rupture of the bladder and trigger premature birth. Otherwise, bacterial vaginosis should be medically investigated if there is any suspicion of subsequent inflammation of the fallopian tubes, cervix and uterine lining. The gynecologist can usually treat the disease quickly and give tips on how to avoid re-infection.
Doctors & therapists in your area
Treatment & Therapy
Spontaneous recovery can be seen in 10 to 20 percent of those with bacterial vaginosis. Otherwise, bacterial vaginosis is treated with antibiotics (metronidazole, clindamycin or nifuratel), which can be administered orally or vaginally and which give positive results in over 90 percent of those affected within a few days.
However, bacterial vaginosis recurs in many cases. Drug therapy is recommended, especially for pregnant women, as untreated bacterial vaginosis increases the risk of premature labor, premature birth and the likelihood of neonatal sepsis.
Preparations containing lactic acid (vaginal suppositories with lactobacilli), glycogen that promotes growth on lactobacilli, and suppositories containing ascorbic acid can help stabilize the vaginal flora. To avoid a “ping-pong effect”, it can be useful to treat your partner as well.
The male genital area can also contain bacterial vaginosis-causing bacteria, but these often do not cause discomfort or altered skin conditions in affected men, so that they can unknowingly cause bacterial vaginosis in women.
Outlook & forecast
The prognosis for bacterial vaginosis depends heavily on the right treatment. Therefore, women who experience symptoms of bacterial vaginosis should definitely see a doctor.
Therapy takes place through the administration of antibiotics. The antibiotic metronidazole, which is usually to be taken orally, is prescribed by default. After about a week, the normal vaginal flora is restored in four out of five patients. However, the recurrence rate for bacterial vaginosis is high, around 60 to 70 percent. Alternative treatments such as topical administration of lactic acid bacteria are less promising.
However, they can help maintain healthy vaginal flora following antibiotic therapy. This may reduce the chance of bacterial vaginosis recurring. Another useful measure is to use condoms during intercourse to avoid re-infection from your partner.
If left untreated, bacterial vaginosis can lead to a variety of complications. These include inflammation of the fallopian tubes, ovaries, uterus, or cervix. In addition, the bacterial imbalance can be the cause of further infections. Bacterial vaginosis can therefore increase the risk of contracting venereal diseases such as chlamydia or even HIV.
prevention
Bacterial vaginosis cannot be prevented directly. However, using a condom during intercourse can minimize the risk of bacterial vaginosis. In addition, excessive vaginal hygiene, which can destabilize the balance of the vaginal flora, should be avoided. The use of probiotic tampons during menstruation and relaxation techniques to minimize psychosocial stress can also reduce the risk of developing bacterial vaginosis.
Aftercare
The bacterial vaginosis is considered to be cured after a scheduled antibiotic treatment and symptom-free treatment. Probiotic pharmaceuticals with lactobacilli, lactic acid or preparations with ascorbic acid are recommended to build up the affected vaginal flora after the administration of antibiotics. These are given intravaginally and help rebuild the vaginal mucosa.
To prevent bacterial vaginosis from recurring, excessive intimate hygiene should be avoided. It is sufficient to clean the genital area with clear water; disposable washcloths available in the drugstore can also be used. It is important to then carefully dry the vaginal area.
Women should also avoid synthetic underwear or panty liners with plastic protection, as this can cause heat build-up and excessive moisture in the genital area. Intimate sprays, soaps and wet wipes are also not recommended for vaginal use, as these can change the pH value of the vaginal environment and thus make the vaginal flora more susceptible to infections.
In addition, care should be taken to clean the anus "from front to back" with toilet paper after using the toilet. This prevents harmful intestinal bacteria from entering the vaginal flora or the urethra and causing infections there again. Women who developed bacterial vaginosis during pregnancy should watch out for any alarm signals even after successful treatment. If you go into premature labor, rupture your bladder, or bleed, you should seek medical help immediately.
You can do that yourself
Lactobacillus cultures are very successful because they restore the bacterial balance. Lactobacilli can also be injected directly into the muscle for a quick effect. The advantage: no hydrogen peroxide is formed, which has a direct effect in the form of antibodies against the harmful bacteria.
A lactic acid regimen with a lactic acid gel over a period of seven to ten days is also promising in most cases. The gel is carefully inserted into the vagina using single-use applicators. In this way, the ideal acidic pH value can be quickly restored.
Even with high doses of vitamin C, for example as a concentrate in powder form with a high bioavailability, the vaginal flora can be restored. It is simply dissolved in water and can be drunk throughout the day.
A Sitz bath with vinegar can kill the bad bacteria, clearing the way for healthy bacteria to colonize. A Sitz bath with a tablespoon of tea tree oil should also be used once a day, this is also a healing home remedy for bacterial vaginosis.
The self-help measures mentioned are not a substitute for treatment by a family doctor or gynecologist. Contacting the doctor for bacterial vaginosis is highly recommended.






















.jpg)

.jpg)
