Patients under a Anosmia have completely lost the ability to perceive smells. None of the more than 10,000 known possible variations of smells can no longer be perceived. The different forms of anosmia are not uncommon.
What is anosmia?

© Axel Kock - stock.adobe.com
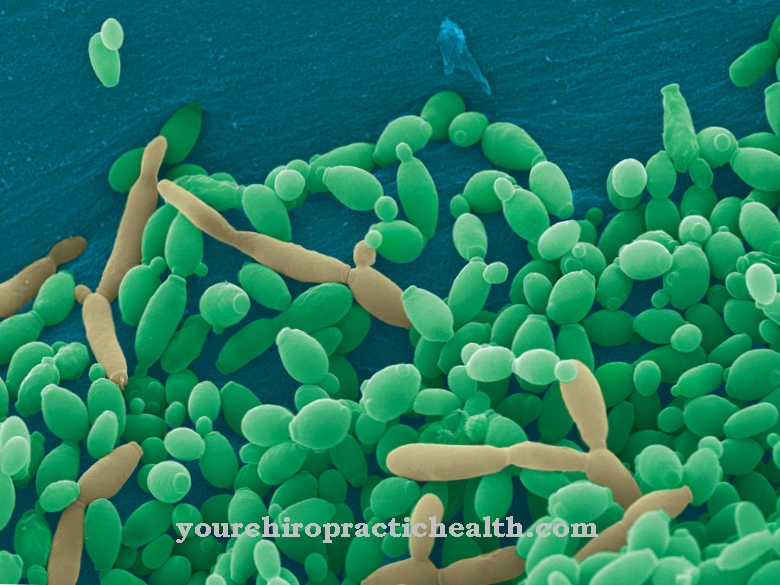
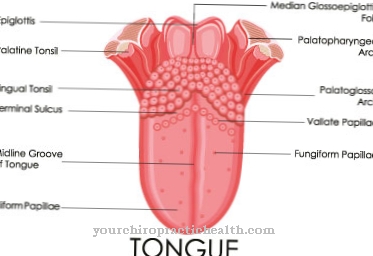
All smells are perceived and processed in the brain, this happens via the so-called olfactory cells in the roof of the nose. From there, the information is passed on as a nerve impulse via the olfactory nerves to the cerebral cortex. In anosmia, this physiological process is either disturbed or can no longer take place at all. How the exact conversion of the olfactory information into olfactory perception takes place in the brain has not yet been finally clarified.
The part of the brain for the perception of smells is also responsible for processing emotions. In everyday life, the lack of odor perception results in various restrictions for those affected, combined with a significantly reduced quality of life. Since the sense of smell is also closely linked to the sense of taste, this also creates problems. For example, if a piece of chocolate is put in the mouth, those affected can only taste the sweetness, but not the fine nuances of the chocolate aroma.
The WHO estimates that tens of thousands of people develop anosmia every year. Depending on the cause, anosmia can be a temporary disorder or a permanent, lifelong limitation. According to the provisions of the Social Security Code, those affected can have a doctor determine a degree of disability from a certain degree of anosmia.
causes
The reasons for anosmia to appear can be very different. In total anosmia, the function of the olfactory nerves has completely failed. No odors can then be perceived at all. If there is a selective anosmia, then those affected can no longer perceive certain smells. Most of the elderly patients do not even notice this clinical picture for a long time.
In addition, a distinction must be made between peripheral and central anosmia, depending on the location and extent of nerve damage:
- If only the olfactory cells are damaged, it is a peripheral anosmia.
- If the odor perceptions in the brain cannot be processed, doctors speak of central anosmia due to the damage to the brain.
The main cause of all types of anosmia is the degeneration of nerve or brain cells with increasing age. Especially after the age of 60, the olfactory ability decreases significantly in both sexes. However, this is a long, rather creeping process. Inhalative smoking and excessive alcohol consumption certainly also lead to a severe impairment of smell. The nerve damage caused by this is fully reversible to a certain extent.
You can find your medication here
➔ Medicines for colds and nasal congestionSymptoms, ailments & signs
The changes are not even noticed for a long time, especially in the weakened peripheral forms of olfactory impairment due to nerve degeneration. With central anosmia, the symptoms can occur more quickly if, for example, tumor growth is the cause.
If there is an obstruction to nasal breathing, the ability to perceive smells is also restricted. Because the gas particles that convey the odor then only partially reach the olfactory cells. In the case of olfactory cell damage, patients complain of malodor, also known as olfactory illusion, as well as a bilateral decline in olfactory ability.
Those affected find this process very uncomfortable. Since the taste perception is always affected in anosmia, those affected often complain of loss of appetite or depressive moods. Your own body odor can also no longer be perceived, which can also lead to social restrictions.
Diagnosis & course
The general practitioner makes the suspected diagnosis and the ENT doctor makes the final diagnosis. To establish the diagnosis, the entire nasal mucosa is examined using a rhinoscope. It is a flexible nasal endoscope with an additional light source so that the doctor can assess the condition of the nasal mucosa.
In addition, the sense of smell must be checked in detail to confirm the diagnosis. This is done subjectively through the presentation of various fragrances and objectively through the method of so-called electronic reaction olfactometry. If central anosmia is suspected, imaging procedures such as CT or MRI are also used.
Complications
Congenital anosmia usually does not result in any complications. Sudden anosmia, on the other hand, is often associated with various problems. First of all, a sudden lack of smell results in a loss of quality of life. The psychological consequences range from depression and anxiety disorders to the fear of unpleasant odor to severe behavioral disorders.
In the long term, anosmia reduces general well-being; the earlier quality of life is usually no longer achieved in the event of a sudden illness. Physically, anosmia can quickly lead to malnutrition and subsequently to deficiency symptoms and other complaints. Food is often too salty or over-seasoned by those affected in order to enhance the taste experience.
This can damage the taste buds, but also various health problems. The lack of a sense of smell also means that there is a risk of poisonous or spoiled food being consumed, which can lead to food poisoning, for example.
There is a danger to life if escaping gases or fires cannot be perceived due to the anosmia. In addition, the lack of the sense of smell in everyday life and at work can lead to problems that often trigger severe psychological and emotional stress. A suddenly occurring anosmia must therefore always be clarified by a doctor.
When should you go to the doctor?
If you suspect anosmia, you should speak to your doctor as soon as possible. Often, a lack of smell is due to a harmless cause that can be quickly diagnosed and treated. However, if it is anosmia, a quick diagnosis is necessary, as a tumor or a degenerative nerve or brain disease may be the cause. Especially people over the age of 60 should see a doctor with olfactory problems.
The ability to smell significantly decreases with age and can cause anosmia in the long term - but this can be treated well if diagnosed in good time. Therefore, especially high-risk groups such as heavy smokers and people who regularly drink alcohol should have a restricted sense of smell examined. Since anosmia is often not noticed immediately by those affected, self-tests are recommended. If the sense of smell or taste is perceived as weakened, a visit to the doctor is advisable. Other contacts are the ENT doctor and, depending on the cause, various internists.
Doctors & therapists in your area
Treatment & Therapy
Treatment of any form of anosmia must always be based on the cause. In many cases, the therapy is considered to be complex and difficult; for a complete healing process, the patient will usually have to be patient. With the essential forms of anosmia, i.e. without a clearly identifiable cause, a self-healing tendency can often be observed. If inflammation or polyps of the nasal mucous membranes or the paranasal sinuses are the cause, the anosmia usually disappears as soon as the inflammatory process has subsided.
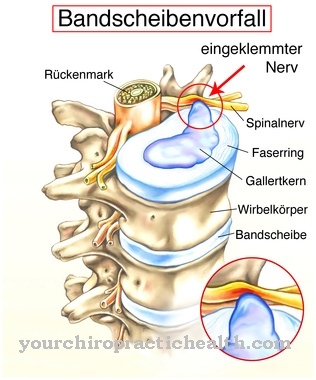
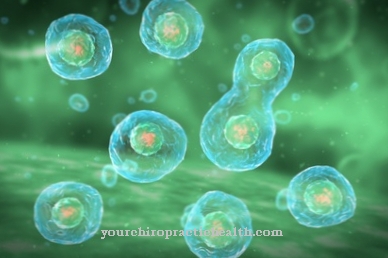
Medicines can also cause severe olfactory disorders as a side effect; in these cases it is necessary to discontinue the medication or replace it with substitute preparations. In the case of central anosmia, it is unfortunately not possible in most cases to regain full olfactory ability due to the irreversible nerve damage. Influenza viruses can also lead to severe, irreversible damage to the olfactory cells and thus to therapy-resistant anosmia.
Outlook & forecast
The prognosis of anosmia depends on its cause and location. If inflammation of the nasal mucous membranes or sinusitis are the reason for the lack of olfactory perception, the chances of those affected are good that their sense of smell will return. Smell perception usually improves on its own after a severe cold. Chronic inflammation of the mucous membranes or allergies can be treated with drugs that reduce swelling. If the anosmia is due to polyps, surgical removal helps to restore the sense of smell.
If the anosmia occurs as a side effect of drugs such as antibiotics, they only have to be stopped. However, if the anosmia was caused by traumatic brain injury, the prognosis is worse. Only about one in five regains their olfactory sense. If there is a central anosmia, for example due to dementia or Parkinson's disease, attention should be directed to the treatment of the serious underlying disease.
According to studies, anosmatic patients who regularly take part in olfactory training have a good prognosis for a complete or at least partial recovery from the olfactory disorder. Experts suspect that olfactory cells grow back after six months of training.
In some cases the anosmia is congenital or the cause cannot be identified. Spontaneous healing is rare, but cannot be ruled out in principle.
You can find your medication here
➔ Medicines for colds and nasal congestionprevention
As soon as an anosmia has been diagnosed, there is a risk for those affected that even dangerous smells from toxic fumes, fire or spoiled food can no longer be perceived. It is therefore helpful to inform family members about the illness.In order to prevent the age-related creeping anosmia, an annual olfactory check can be useful in suspected cases. In order to prevent anosmia caused by stimulants, alcohol and nicotine consumption should be avoided.
Aftercare
The extent to which follow-up care is necessary depends on whether the sense of smell could be restored through initial therapy or not. If the outcome is positive, there should be no more complaints. Aftercare is not required. However, this does not mean that the anosmia cannot arise a second time. There is no immunity. The known causes can again cause a loss of smell.
The situation is different if those affected do not get their sense of smell back completely or not at all after an initial treatment. Depending on the cause, doctors may administer medication or perform another operation. Scientists assume that human olfactory cells grow back if they are adequately trained. In addition, patients receive so-called smelling pens, which they have to sniff at several times a day.
The anosmia cannot be prevented by preventive measures. Follow-up care cannot begin at this point. Rather, it tries to remedy the causes of the loss of smell by means of suitable methods and to restore the sense of smell with suitable therapy. If there is no success, it has serious consequences for the sick. It is no longer possible to enjoy food as usual. Many stimuli are missing in social contact.
You can do that yourself
The loss of the sense of smell significantly reduces the quality of life and can even be dangerous in some situations. Often the importance of the sense of smell for coping with everyday life is underestimated and only the stimulating sensory perception is missed.
However, those affected must realize that they can no longer identify contaminated food as they used to. Great care is therefore required when storing perishable food. If in doubt, food should be disposed of as food poisoning can be very dangerous.
People who live alone or are regularly alone at home should also bear in mind that they can no longer perceive an apartment fire olfactorily. It is therefore important to install a sufficient number of smoke alarms and to check their functionality regularly.
Affected people are often unsettled in their social interaction with others because they can no longer perceive whether they smell of sweat on hot summer days, suffer from bad breath or have used too much perfume or after shave. Here, those affected should look for someone they can trust at work or in other groups in which they move regularly, who can point out a possible faux pas.



.jpg)
.jpg)












.jpg)
.jpg)