Baroreceptors are mechanoreceptors in human arteries and veins that regulate blood pressure. They are connected to the medulla oblongata and register changes in blood pressure and heart rate. By keeping blood pressure constant, they play an important role in maintaining blood circulation.
What is a baroreceptor?
The most important sensory cells of the sense of touch are the mechanoreceptors. These receptors are the first point of contact for the perception of external pressure stimuli. In addition to exteroceptive tasks, mechanoreceptors also perform tasks in interoception and thus also detect pressure stimuli within the human body.
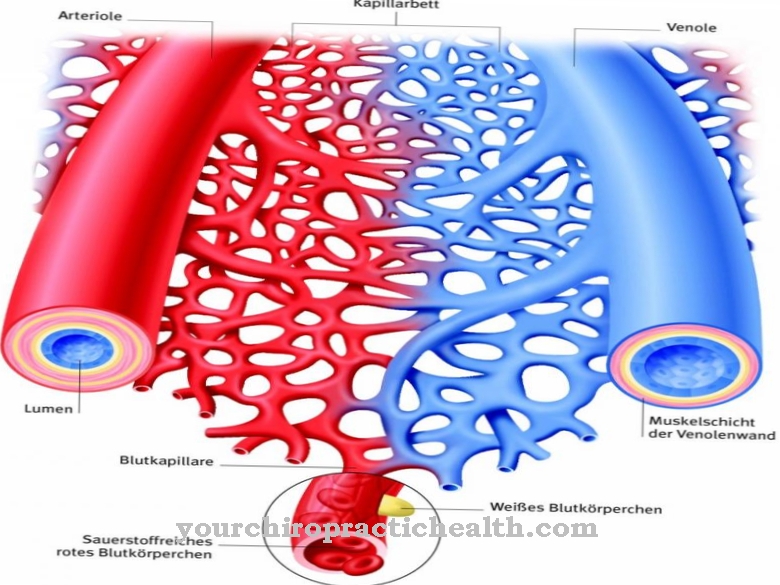
The presso- or baroreceptors are mechanoreceptors of interoception that sit in the wall of the human blood vessels. They continuously collect information about blood pressure in the arteries and veins. Depending on their location, baroreceptors can be divided into arterial and venous receptors. Arterial baroreceptors are also called high pressure baroreceptors. They can be assigned to the proportional-differential receptor group.
Venous baroreceptors are called low pressure baroreceptors. The sensory cells in the blood vessels are the main body that mediates adjustments in cardiac output and total peripheral resistance. The regulation of the blood volume also falls within their area of responsibility.
Anatomy & structure
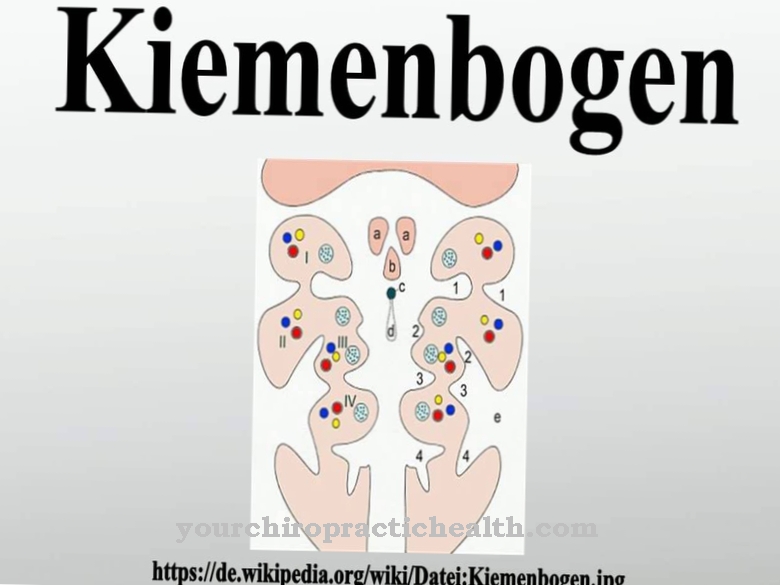
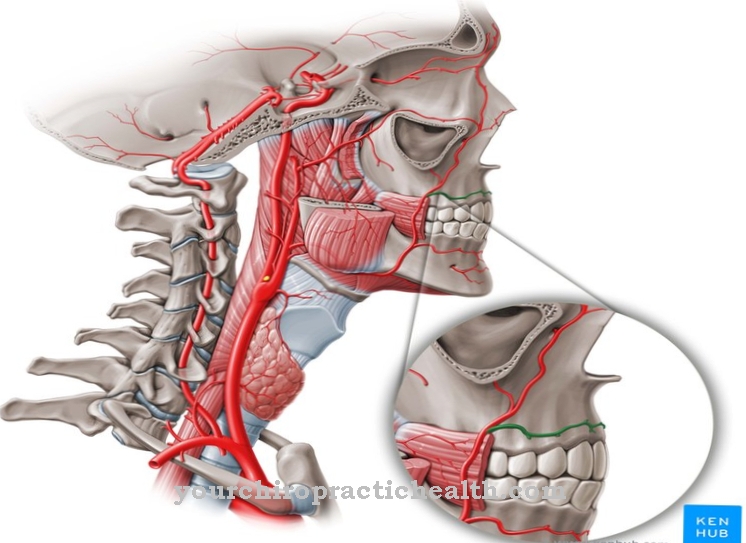
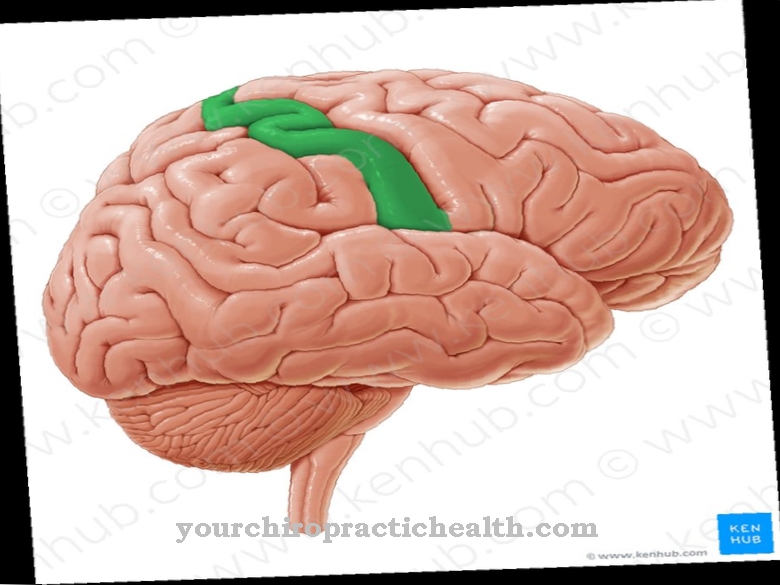
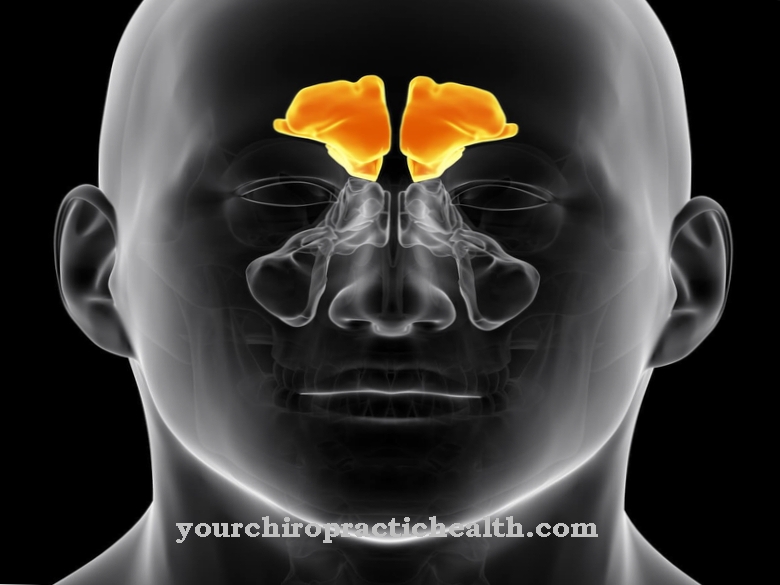
Arterial baroreceptors are mainly located in the aortic arch and the carotid sinus. The density of pressoreceptors in the other body arteries is significantly lower compared to these structures. In the border area between the arterial baroreceptors there are, from a histological point of view, intertwined nerve fibers that have an oval, lamellar end organ.
These sensory cells are proportional-differential receptors and therefore register changes in blood pressure as well as the value of the mean blood pressure. Their discharge rate is not based on absolute values. If the mean blood pressure changes permanently, the receptors adapt to the new base values. Due to their ability to adapt, the receptors report the change after a change in blood pressure, but no longer send any signals if the blood pressure changes continuously.
Function & tasks
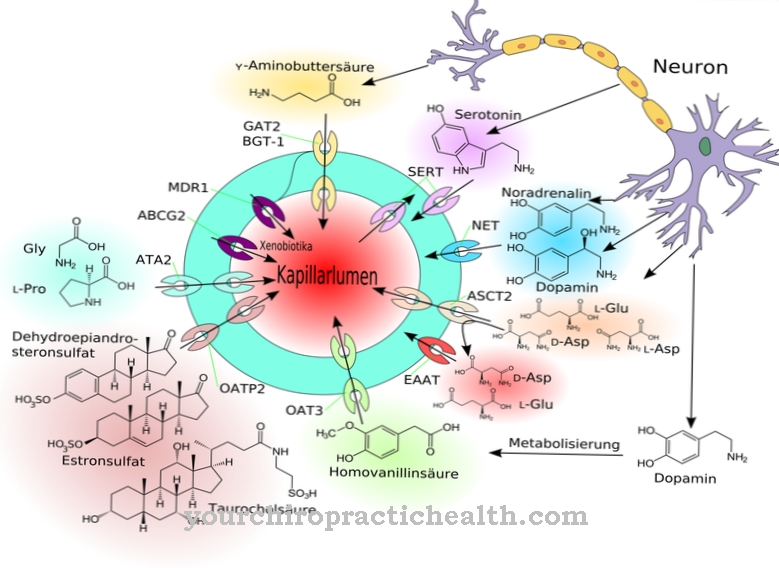
In addition to the information mentioned, the sensory cells permanently collect information on the rate of change, the blood pressure amplitude and the heart rate. This information is forwarded to the circulatory center of the medulla oblongata as an action potential proportional to the stimulus acting on it, where the blood pressure is regulated by means of negative feedback.
The nerves of the baroreceptors extend afferently over the X or IX nerve to the brain stem, where they project onto the nucleus tractus solitarii. The activity of the baroreceptors can be traced by means of the baroreceptor reflex. This reflex corresponds to the baroreceptive response to changes in blood pressure. A rise in blood pressure activates the parasympathetic nerve via the vagus nerve and at the same time causes the sympathetic nerve to drop. This creates a negative chronotropic effect on the heart and the peripheral resistance vessels are dilated. If, on the other hand, the blood pressure drops, an inhibition of the parasympathetic tone is set in motion, the heart rate increases and the total peripheral resistance increases due to a contraction in the resistance vessels.
At the same time as this reaction, there is an increase in the venous return flow. Venous baroreceptors are located in the veins of the body instead of arterial ones. Their density is highest in the large body veins and in the right atrium. These sensory cells are not presso but rather stretch receptors and regulate blood volume. Above all, the arterial baroreceptors are vital as they keep arterial blood pressure constant and ensure the blood supply to the organs as required. For example, if the blood pressure drops sharply after a hypovolemic shock, the aortic wall hardly expands.
The signal frequency of the pressoreceptors to the medulla oblongata decreases in this way and the neurons of the medulla oblongata can send regulatory signals to the heart muscle. The activity of all baroreceptors is permanent and thus primarily fulfills circulatory-regulating tasks.
You can find your medication here
➔ Medicines for balance disorders and dizzinessDiseases
The baroreflex is medically relevant to the highest degree and is primarily associated with circulatory diseases and fluctuations in blood pressure. Everyone's circulatory system is exposed to high levels of stress every day.
1000 milliliters of blood migrate from the legs into the abdomen when you simply stand up from a sitting or lying position. An intact baroreflex keeps the blood pressure and heart rate constant with minor fluctuations despite these stresses when getting up and lying down. However, if there is damage to the nerves involved in the heart, blood vessels or kidneys, what is known as autonomous failure occurs. This phenomenon is also called autonomic neuropathy. The blood pressure of those affected drops sharply when they stand up and circulatory problems or even fainting occur.
Long-standing diabetes, for example, can be responsible for such nerve damage. The baroreceptors themselves can also be affected by damage, for example in the context of severe poisoning. Patients with damaged baroreceptors or lesions of the nerve pathways to the brain are often affected by extreme fluctuations in blood pressure. Even the smallest effort or excitement can get your blood pressure up. In this context, the doctor speaks of baroreflex failure. A disruption or failure of the baroreflex can lead to secondary diseases.
Above all, defective baroreceptor functions have an effect on the course of chronic cardiovascular diseases, especially high blood pressure. The baroreflex can be examined invasively or non-invasively in order to prevent secondary diseases. When examining the reflex, the doctor usually measures the changes in the heart rate, which can be provoked by a controlled change in blood pressure. Strong disturbances of the baroreceptor reflex can cause cardiovascular failure. In extreme cases, this can result in cardiac death.



.jpg)