At Bilirubin it is a breakdown product in the hemoglobin metabolism. Macrophages continuously break down old erythrocytes in the liver and spleen and thus generate bilirubin. If this process is disturbed, the substance is deposited and jaundice develops.
What is bilirubin?
Bilirubin is the breakdown product of the red blood pigment. This dye is also known as hemoglobin. Red blood cells only live around 120 days. The renewal and excretion of old erythrocytes takes place in the form of hemoglobin metabolism. Macrophages permanently break down old erythrocytes, especially in the spleen and liver. In the context of the so-called haem oxygenase, hemoglbin becomes the intermediate stage biliverdin, which results in bilirubin in biliverdin reductase.
The bilirubin binds to albumin in the blood plasma. The degradation product is yellowish-brown in color and 90 percent of the blood is bound to albumin. In the case of albumin-bound bilirubin, primary bilirubin is also used. Conjugated bilirubin, on the other hand, is produced in the liver cells, where the substance couples to glucuronic acid. Together, conjugated and unconjugated bilirubin make up direct bilirubin. Around 30 milligrams of bilirubin are produced in the human body every day. A large proportion of it is excreted via the intestines and urinary tract.
Anatomy & structure
Bilirubin is always a bile pigment. There are several types of it that differ anatomically. The main distinction arises from the different pathways of blood metabolism, which have been mentioned above. Indirect bilirubin is non-covalent and is bound to albumin. This is the primary and unconjugated portion of bilirubin.
Direct bilirubin, on the other hand, is glucuronidated and corresponds to the conjugated, secondary bilirubin. Delta bilirubin, which is covalently bound to albumin, also falls into this group. A covalent bond is used for all chemical bonds that have shared electron pairs between the molecular atoms. The bilirubin of animals and plants has a similar structure to that of humans. Only direct bilirubin is clinically measurable. The indirect part is usually calculated from the direct part.
Function & tasks
In the human body, bilirubin itself does not actually take on any functions or tasks. By and large, this applies to almost all breakdown products. In contrast, the starting product hemoglobin even takes on vital functions in the human organism. The red blood pigment mainly transports oxygen and carbon dioxide. Each hemoglobin molecule is thus equipped with four oxygen molecules.
In this way, oxygen only reaches the lungs and tissues of the body. Due to its ability to bind to nitric oxide, hemoglobin also regulates blood pressure. When the nitric oxide is released from the hemoglobin molecules bound to it, the blood vessels, for example, expand. The blood circulation improves and the blood pressure decreases. Without the red blood pigment, no life would be possible, since the vital transport of oxygen could not take place. After a lifetime of 120 days, red blood cells die doing these vital tasks and new ones follow. For this to happen, the old blood cells have to be broken down and excreted.
So bilirubin is just a degradation product of the blood pigment that makes old erythrocytes excretable. If the bilirubin were no longer excreted, it would be stored. This phenomenon turns the skin yellowish. The liver is particularly responsible for breaking down the substance. The bilirubin value can therefore give laboratory diagnostic indications of a liver disease. An increased value can also indicate a backlog of the bile. In addition to these possible causes, a number of different syndromes are also associated with elevated bilirubin levels.
Diseases
One of the most well-known bilirubin-related diseases is jaundice. With this phenomenon, the substance is stored. With this phenomenon, the serum bilirubin value is above 1.2 mg / dl. First the white skin of the eyes turns yellow due to the deposits. Later on, the rest of the skin is also affected. Jaundice with greatly increased concentrations of the breakdown product even discolor the organs yellow.
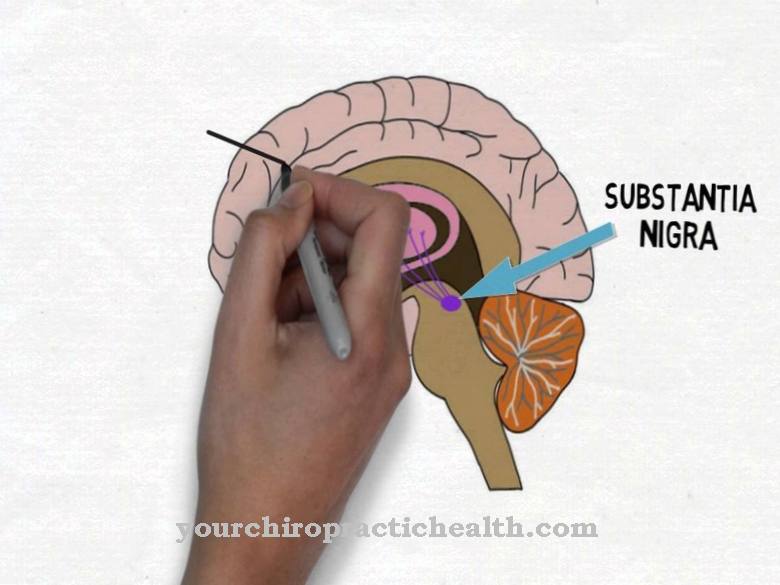
Newborn jaundice is most common because newborns break down fetal hemoglobin, which can lead to increased bilirubin levels. Because the blood-brain barrier is not fully developed in the newborn, this form of jaundice can also lead to development-impairing deposits in the cerebrum or in the basal ganglia. Jaundice at a later age can have various causes. For example, jaundice can occur in the context of Dubin-Johnson syndrome or Rotor syndrome. The same is true of Gilbert syndrome and Crigler-Najjar syndrome, an inherited metabolic disease of hemoglobin.
All liver diseases are also frequently associated with jaundice. Extreme liver stress from poisoning or alcohol addiction can lead to jaundice, for example. The same applies to liver inflammation or liver metastases from tumors. The causal therapy procedure differs with the cause of the jaundice and the increased bilirubin level. In the case of disorders of the hemoglobin metabolism, symptomatic treatment generally corresponds primarily to the breakdown of the stored bilirubin. In the meantime, there are promising therapeutic options available for breakdown from the skin. The stored degradation product can be converted into lumirubin using phototherapy. This substance is soluble in water and can therefore be excreted.




















.jpg)



