Francisella tularensis is the causative agent of the infectious disease tularemia. The pathogen is a rod bacterium from the Pasteurellacae family.
What is Francisella tularensis?
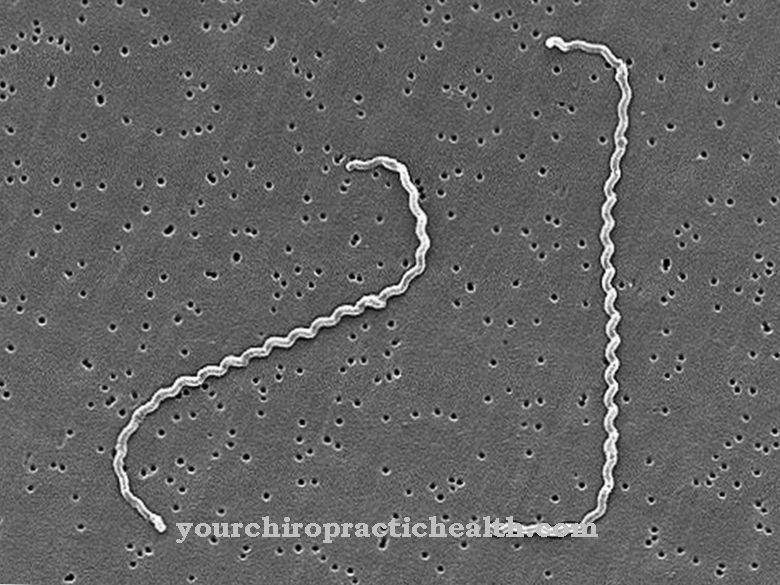
The Francisella tularensis bacterium is a gram-negative pathogen. In contrast to gram-positive bacteria, gram-negative bacteria also have an outer cell membrane in addition to the thin peptidoglycan layer made of murein. The pathogen Francisella tularensis is pleomorphic. Pleomorphic bacteria are multifaceted. They change their cell shape depending on the environmental conditions. Their appearance also depends on the stage of development.
Francisella tularensis belongs to the coccoid rod bacteria. Rod bacteria are actually elongated, whereas the cocoid rod bacteria are somewhat rounded. There are four different subtypes of the pathogen. However, the three clinically important forms are identical in serology. Two groups of Francisella tularensis can be distinguished biochemically and genotypically. The bacterium Francisella tularensis biovar tularensis from Jellison type A is highly virulent and causes severe disease that is often fatal. The bacterium Francisella tularensis biovar holarctica of Jellison type B is less virulent. But this bacterium can also cause serious diseases.
Occurrence, Distribution & Properties
Francisella tularensis is native to Scandinavia, Russia, China, Japan, USA and Canada. Francisella tularensis biovar tularensis type A is mainly found in North America. Francisella tularensis biovar palaearctica occurs worldwide. Pathogen reservoirs are hares, rats, squirrels, mice and rabbits. But the pathogen can also be found in the earth and in water. The small mammals become infected either through contact with contaminated water or soil material or through blood-sucking parasites such as flies, ticks or mosquitoes.
The bacterium is transmitted to humans through contact with the mucous membrane or skin of contaminated animal material. Eating inadequately heated, infectious meat is also a possible source of infection. In particular, the consumption of rabbit meat has proven to be a possible route of infection. Inhaling contaminated dust (e.g. from hay, straw or earth) can also lead to infection. The same applies to contact with infected mosquitoes, ticks or flies.
The infection cannot be transmitted from person to person. However, when handling pathogens or inhaling aerosols containing pathogens, people can become infected in the laboratory. The rural population is more often affected by an infection with Francisella tularensis. The infection here mostly occurs through the processing of game meat or other agricultural products.
The pathogen Francisella tularensis is highly contagious. This means that even smaller amounts of pathogen are sufficient to trigger an infection. The incubation period is three to five days. Depending on the dose of infection, the route of infection and the virulence of the pathogen, the incubation period can be up to three weeks.
Illnesses & ailments
Tularemia is a reportable zoonosis. Although the disease is rather rare, it is often severe and life-threatening. A distinction can be made between an external (localized) and an internal (invasive) form.
The external ulceroglandular form is the most common form of tularemia. It starts very suddenly with a sharp rise in fever. Ulcers form at the point of entry of the pathogen. The local lymph nodes are inflamed with pus. In oculoglandular tularemia, also known as parinaud conjunctivitis, the entry point of the pathogen is at the conjunctiva of the eye. It can be seen as a yellow knot. In the eye, the pathogen causes a painful inflammation of the conjunctiva (conjunctivitis). The lymph nodes on the neck and in front of the ear are swollen.
In glandular tularemia, no portal of entry can be seen. The formation of ulcers also does not occur. Only the regional lymph nodes are swollen and painful. Glandulopharyngeal tularemia is found mainly in children. This is where ulcers form in the oral cavity and throat. The lymph nodes in the corner of the jaw are swollen.
When the pathogens are inhaled or reached the internal organs via the bloodstream, the internal or invasive form of the disease develops. Typhoid tularemia occurs primarily when slaughtering or working in the laboratory. The lungs and airways are often affected. Patients have a high fever and headaches and sweats. Lung abscesses are a dreaded complication of typhoid tularemia. In addition, the meninges (meningitis) can become inflamed. Inflammation of the middle layer (mediastinitis) or the pericardium (pericarditis) is possible. Other complications are rhabdomyolysis and osteomyelitis. Typhoid tularemia is also known as septic or generalized tularemia. It is very dangerous and has a high mortality rate.
Intestinal tularemia probably develops from the consumption of contaminated meat that has not been adequately heated. Typical symptoms are vomiting, nausea, sore throat, diarrhea and pain in the abdomen.
The second most common form of tularemia is pulmonary tularemia. It manifests itself in the form of inflammation of the lungs (pneumonia). Patients have cough with phlegm, shortness of breath, and chest pain. The abdominal tularemia shows a typhoid-like clinical picture. The liver and spleen are swollen. The patients suffer from diarrhea and abdominal pain.
Tularemia is treated with antibiotics. Streptomycin in particular has been shown to be effective. There is resistance to penicillin and sulfonamides. Even with antibiotic treatment, five percent of all invasive forms are fatal. Without treatment, the mortality rate is over 30 percent. The mortality of the American forms of tularemia is significantly higher than that of the European strains of Francisella tularensis.























.jpg)


