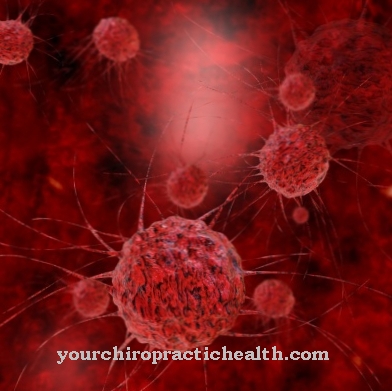
Blood in the stool is mostly caused by inflammation and internal injuries to the gastrointestinal tract. But other diseases such as hemorrhoids, colon cancer or colon polyps can cause blood in the stool.
What is blood in stool?

If blood is excreted in the stool with daily bowel movements or if the stool is covered or deposited with blood, internal bleeding in the gastrointestinal tract can usually be assumed. This symptom should not be taken lightly, but should be clarified by a doctor.
Medically, blood in stool can be divided into four categories:
Hematochezia:
There are red or light red blood deposits on the stool. This gastrointestinal bleeding usually originates from the lower sections of the intestine, upper sections of the digestive tract or from ruptured hemorrhoids.
Occult blood in the stool:
With this type of blood in the stool, the blood in the stool is not visible, but is mixed with the stool. In order to actually determine the blood, a hemoccult test by the doctor is necessary.
Blood stool:
In the so-called blood stool, the stool is mixed with dark and light blood.
Tarry stool (Meläna):
In this form, the stool is very dark to black in color and sometimes smells pungent and foul. This is where bleeding occurs in the upper digestive tract and is also known as upper gastrointestinal bleeding.
causes
While there are some serious diseases (such as colon cancer) that involve blood in the stool, most of the causes are harmless. Nevertheless, if there is blood in the stool, a doctor should always be consulted to determine the exact cause.
The more harmless causes include the well-known hemorrhoids, in which mainly bright red blood deposits are visible. Fissures (tears in the mucous membrane) can also be the cause. These cracks can occur in the context of chronic intestinal inflammation, such as Crohn's disease or ulcerative colitis. Mucous membrane tears are also possible in the course of anal intercourse.
In addition, intestinal polyps, intestinal diverticula, vascular inflammation and rare blood disorders for blood around stool are also possible. Sometimes parasites or intestinal infections can also cause intestinal bleeding. The well-known gastric ulcer (ulcus ventriculi) can also turn the stool black.
Diseases with this symptom
- Mesenteric infarction
- Intestinal polyps
- Small bowel cancer
- Duodenitis
- Stomach cancer
- Ulcerative colitis
- abdominal influenza
- Diverticulitis
- Reflux esophagitis
- hemorrhoids
- Crohn's disease
- Tarry stool
- Colon cancer
- Colon polyps
- Mallory-Weiss Syndrome
- Esophageal variceal bleeding
- Duodenal ulcer
- Gastric ulcer
Complications
Blood in stool almost always has serious causes. Diagnosing this cause can take some time, however - enough time for complications to arise. For example, if the blood in the stool is cancer of the bowel, there is a risk that the severity of the disease will not be recognized by then.
If it is at an advanced stage, the tumor may have already perforated the intestinal wall - as a result, serious internal bleeding will occur if the tumor continues. This requires immediate emergency surgery, since the loss of blood in such internal injuries is not insignificant. The same thing can happen with another cause of blood in the stool, namely hemorrhoids. These are not only uncomfortable and painful, they can also lead to high blood loss if the injuries to these blood vessels become more serious.
Hemorrhoid patients already know blood in their stool and sometimes no longer take it seriously, even if it is more than usual. However, doing so could quickly make them overlook if there is a more serious hemorrhoid injury that needs medical attention. In order to avoid complications, a doctor should always be consulted if there is blood in the stool and changes should be taken seriously, especially if there is more blood in the stool than usual, even if a diagnosis has been made.
When should you go to the doctor?
Basically: Blood in the stool is not to be trifled with. It is better to see a doctor as early as possible. Most bleeding stops by itself without the intervention of a doctor. However, the cause of the bleeding should be clarified in order to be able to initiate treatment if necessary and to rule out serious illnesses.
This applies in particular to recurring incidents that cannot be traced back to a specific activity with a probability bordering on certainty. A doctor must be consulted immediately if, in addition to the blood in the stool, other symptoms such as pain, nausea, vomiting, a feeling of exhaustion and tiredness occur.
The first point of contact is a general practitioner. If necessary, they can refer you to a specialist such as a proctologist. He specializes in diseases of the rectum, rectum and anal canal. If it is suspected that anal fissures or similar injuries are not the reason for the blood in the stool, other internists can also be considered.
Only in individual cases does it make sense to observe your own bowel movements for a certain period of time. This can be the case with marginal bleeding, which is almost certainly due to a certain external activity. However, a visit to the doctor must be followed if there is no improvement after a short time.
Doctors & therapists in your area
Treatment & Therapy
Blood in the stool usually requires a medical examination and diagnosis to rule out dangerous diseases. The medical examination will mainly try to find out where and where the bleeding occurs in the gastrointestinal tract.
A sample of the stool can also provide initial clues, through color and consistency, of a possible cause. The so-called haemoccult test, as a stool blood test, comes into question here. With its help, the doctor can biochemically detect the blood in the stool if it is not directly visible to the naked eye.
Once the bleeding site has been found and the cause identified, the bleeding must be stopped. Rapid intervention is necessary, particularly in the case of gastric ulcers or bleeding from varicose veins in the escalator. Any further treatment then depends on the course or other causes of the disease. Hemorrhoids are usually treated with suppositories and ointments. Colon polyps may need to be surgically removed. For colon cancer, surgery with chemotherapy is also often necessary.
Outlook & forecast
Blood in the stool is definitely an indicator of illness. How this disease will progress over time with and without medical treatment can only be determined once the cause of the bleeding has been clearly clarified.
If the person concerned only perceives very small amounts of blood in the stool, there is a very high probability that they have haemorrhoidal disease. Small fissures in the gastrointestinal tract can also cause less bleeding in the stool. Without medical treatment, this clinical picture should go away on its own. After around two to three days, these small injuries heal completely by themselves, so that a serious course of the disease can be excluded.
However, caution should be exercised if the amount of blood in your stool increases. Such a symptom can be a sign of internal bleeding. If these are left untreated, this can lead to death. There is also the possibility that the person affected has colon cancer. This is mainly noticeable through regular bleeding, which can be seen in the stool within a short time.
If such symptoms are identified and treated at an early stage, the prognosis for a full recovery is very likely. Therefore, if you notice blood in your own stool, you should definitely have it checked by a doctor.
You can find your medication here
➔ Medicines for digestive problemsYou can do that yourself
If there is blood in the stool, the patient can do some things himself. With regard to hemorrhoids, suppositories and ointments have proven effective. Witch hazel ointment helps in mild cases, and cortisone suppositories in severe cases. Many ointments - including witch hazel ointment - have an astringent (contracting) effect, which ensures that smaller vessels close. Sitz baths with oak bark also help. The tannins of the oak bark have an itch-relieving, slightly anti-inflammatory and astringent effect.
For hemorrhoids, diverticulosis, ulcerative colitis, and Crohn's disease - all possible causes of lower digestive tract bleeding - high-fiber diet and exercise are effective. If the stool becomes softer, less pressure builds up in the bowel. Causes of blood from the upper digestive tract are mostly inflammatory processes in the stomach or esophagus. In acute cases, a light diet is sufficient for gastritis. A lot of fluids and the avoidance of substances irritating the gastric mucous membranes - coffee, alcohol and carbonated drinks - are beneficial.
Antacids work for gastric ulcers. Coffee and tobacco should also be avoided if you have stomach ulcers. A proven home remedy is cabbage juice in raw food quality, available e.g. in health food stores. Stress reduction and relaxation exercises also help with stomach ulcers. Proton pump inhibitors, which reduce acid production in the stomach, are prescribed for esophagitis. Healing clay and base powder are recommendations of naturopathy.










.jpg)