As Bourneville-Pringle Syndrome a triad of tumors of the brain with epilepsy and developmental delay, skin lesions and growths in other organ systems is known. The disease is caused by a mutation of the two genes TSC1 and TSC2. Therapy is symptomatic with a focus on epilepsy.
What is Bourneville-Pringle Syndrome?

© Henrie - stock.adobe.com
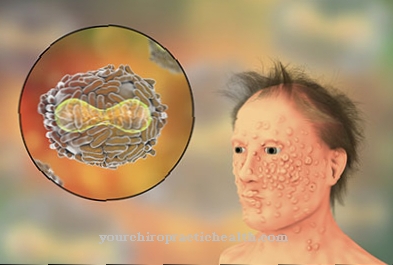
The medical term Bourneville-Pringle syndrome is a synonym for the tuberous sclerosis. This pathological phenomenon falls into the group of hereditary diseases and is characterized by mostly benign tumors on the face, in the brain and in the organ system, by intellectual disabilities and epileptic seizures.
The prevalence of tuberous sclerosis in newborns is around one case in 8,000 infants. The French neurologists Désiré-Magloire Bourneville and Édouard Brissaud first described the disease together with the British dermatologist John James Pringle in the 19th century. The name Bourneville-Pringle Syndrome has come into being for their sake.
In the English-speaking world, the symptom complex is called Tuberous Sclerosis Complex. Clinically, the complex is characterized by a symptomatic triad with the symptoms mentioned above. A special form of the syndrome is the contiguous gene syndrome.
causes
Familial clusters have been observed in connection with Bourneville-Pringle syndrome, apparently based on an autosomal dominant inheritance. In half of all cases, however, the disease is apparently based on a new genetic mutation as the cause. The rate of spontaneous mutations is thus at least as high as that of inherited mutations.
In familial cases, mutations in the TSC1 gene on locus Chr.9q34 and in the TSC2 gene on locus Chr.16p13 were observed with the same frequency. The sporadic occurrence is almost exclusively limited to new mutations in the TSC2 gene. Both genes are tumor suppressor genes and are therefore involved in suppressing cell growth. Their gene products are hamartin and tuberin, the functions of which have not been conclusively clarified.
The mutations in the context of a Bourneville-Pringle syndrome are distributed over all exons of the genes mentioned and can correspond to any type of mutation. Only large deletions in the TSC2 gene on one or more exons have not yet been observed. The special form of the contiguous gene syndrome affects both the TSC2 gene and the PKD1 gene.
Symptoms, ailments & signs
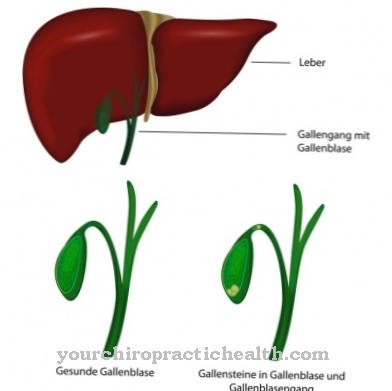
Tuberous sclerosis is characterized by multiple areas of abnormal tissue differentiation, called hamartiae, that vary in location with respect to the organ systems. The main criteria of the disease include facial angiofibromas and connective tissue nevi in the forehead area, non-traumatic angiofibromas, at least three hypomelanotic spots, connective tissue nevi of the sacrum and several hamartomas on the retina.
In addition to cortical dysplasia, there are also subependymal nodules, subependymal giant cell symptoms and rhabdomyomas of the heart. In addition, pulmonary lymphangiomyomatoses and angiomyolipoma of the kidneys can be named as the main criteria. Accompanying symptoms, the patients usually have tooth enamel defects, rectal polyps or osseous cyst formations.
In addition, symptoms may be accompanied by an unusual stiffening of the white matter of the brain. The same applies to gingival fibroids, depigmentation and cysts of the kidneys. The triad of the syndrome is divided into symptomatic skin changes, malformations of the brain with developmental disorders and epilepsy and symptoms of other organ systems.
Diagnosis & course
To diagnose tuberous sclerosis, the doctor shows the patient either two main criteria of the disease or one main symptom with two secondary criteria. The changes in the brain are usually detected the earliest and are usually shown using imaging such as an MRI. A molecular genetic analysis can confirm the suspected diagnosis of the syndrome and rule out similar syndromes from a differential diagnosis.
The prognosis is good for patients with rather mild Bourneville-Pringle syndrome. Many patients with mild BPD lead mostly normal lives. People affected by severe BPD and thus severe epilepsy, extreme cognitive impairment and a large number of tumors have a poorer prognosis and may have to expect life-shortening effects.
Complications
In Bourneville-Pringle syndrome or tuberous sclerosis, different organ systems are affected and can have different complications. On the one hand, this disease mainly affects the central nervous system and the brain. Those affected suffer from epilepsy, especially in childhood. Partial seizures are the most common, but they can also be generalized.
If left untreated, childhood epilepsy can develop into Lennox-Gausaut syndrome. The person concerned suffers a mostly tonic seizure and absences several times a day, which in the worst case can turn into a status epilepticus, a medical emergency. Sometimes mental development disorders can also be observed in the child.
Furthermore, one patient can develop increased intracranial pressure in the course of the disease. This leads to severe headaches and impaired consciousness. In the worst cases, important control centers can become trapped in the area of the elongated medulla (medulla oblongata), which can lead to respiratory failure.
Tuberous sclerosis can also be the cause of kidney cysts or malignant tumors, which can be responsible for kidney failure (renal insufficiency). This severely limits the quality of life and the patient may have to undergo dialysis or a transplant. Intracardiac rhabdomyoma can develop in the heart, which can be responsible for cardiac arrhythmias or even cardiac death.
When should you go to the doctor?
If epileptic seizures and cognitive impairment persist, a doctor should be consulted. He can use an ultrasound examination to determine whether Bourneville-Pringle syndrome is the cause. A targeted diagnosis of the tumor disease is only possible after a comprehensive anamnesis. The characteristic epilepsy can already be determined in the first months of life.
The pediatrician will then arrange for a routine examination and quickly diagnose Bourneville-Pringle syndrome. If the epileptic seizures do not occur, the diagnosis is more difficult. Any developmental disorders and behavioral problems often only develop in the course of childhood or adolescence. Basically: if the child behaves abnormally, has difficulties learning or shows other impairments, the pediatrician must be consulted.
Other warning signs that require medical clarification are increasing skin changes such as reddish poplars or the characteristic leaf-shaped spots on the skin. In the further course, skin tumors, lumps and other abnormalities can appear. If one or both parents have Bourneville-Pringle syndrome, it is advisable to get a medical evaluation during pregnancy.
Doctors & therapists in your area
Treatment & Therapy
So far, Bourneville-Pringle syndrome cannot be treated causally, since only gene therapy approaches can be considered as causal therapy and these approaches are currently the subject of research, but have not yet been approved for use. For this reason, only symptomatic therapies are currently available for treatment.
The therapy of epilepsy is the focus of the therapy, since it is precisely this symptom that severely impairs the quality of life of those affected and, in the worst case, causes a severe deterioration in the state of health up to death. Epilepsy treatment is either medicated or, in severe cases, surgically as far as possible.
For example, the separation of the two brain hemispheres through the surgical removal of the corpus callosum has shown success in epilepsy therapy in the past. For milder forms, the administration of anti-epileptics is often sufficient. In addition to these treatment steps, the tumors must be removed from the organ systems. As these are mostly benign tumors, subsequent irradiation is usually not indicated.
In the case of the large number of tumors, however, close monitoring is indicated in order to identify possible changes leading to malignant ones in good time. Since those affected often suffer from mentally retarded development, measures such as early intervention can also be appropriate therapeutic steps. Speech development can be supported by speech therapy.
The motor development delays can be countered with physiotherapy and occupational therapy measures. If the illness results in psychological stress for the patient, psychotherapy can also be useful.
Outlook & forecast
There is currently no curative therapy for Bourneville-Pringle syndrome. Only symptomatic treatment is possible. The severity of the disease is different for each patient. As a rule, life expectancy is normal. However, this can be reduced by frequent epileptic seizures, severe mental retardation and malignant degeneration of the existing tumors.
The therapy is particularly limited to the treatment of epileptic seizures. As part of the disease, all types of seizures occur in epilepsy. An association between cognitive development and the frequency of seizures has been observed. Adults mainly experience secondary generalized focal seizures.
Overall, there are developmental disorders that manifest themselves in language, movement and learning disorders. The intelligence quotient of the individual affected can develop differently. While this is normal in half of the patients, around 31 percent of the patients achieve a quotient of a maximum of 21.
The skin changes are also different and depend on age. These are sebum adenomas. The cosmetic treatment of the adenomas is carried out by surgical removal or laser irradiation. Often there is also an angiomyolipoma, a benign tumor in kidney tissue. A benign tumor can also develop in the striated muscles of the heart. Other organs such as the lungs can also be affected by tumors. Malignant degeneration is very rare.
prevention
So far, Bourneville-Pringle syndrome can only be prevented if, in family planning, couples can use molecular genetic tests to assess their risk for sick children and, if there is an increased risk, decide against having their own children.
You can do that yourself
Tuberous sclerosis, also known as Bourneville-Pringle syndrome, is a genetic disease that cannot yet be treated causally. Therapeutic measures therefore start with the symptoms.
Epilepsy is one of the most troublesome side effects that usually severely impair the quality of life of those affected. In addition to the drug treatment with anti-epileptic drugs, those affected can often contribute to the fact that the seizures occur less frequently or are less severe through their lifestyle. Patients should keep an epilepsy diary to find out whether factors in their everyday life are triggering the seizures.
Such factors can be entirely different in nature. Certain foods, alcohol, mind-altering drugs as well as lack of sleep, stress, severe feelings of anxiety or, in women, menstrual periods. Critical factors should be avoided as far as possible. Many sufferers and their relatives also benefit from joining a self-help group for epileptics, which now exists in numerous German cities.
Very often, those affected by tuberous sclerosis also suffer from retarded intellectual development. The negative consequences can be counteracted by adequate early intervention. Parents can get advice from paediatricians or the youth welfare office. If the development of motor skills is also impaired, occupational and physiotherapeutic measures help. In the case of delayed language development, a speech therapist should be consulted.

.jpg)
.jpg)
.jpg)
.jpg)

















.jpg)



