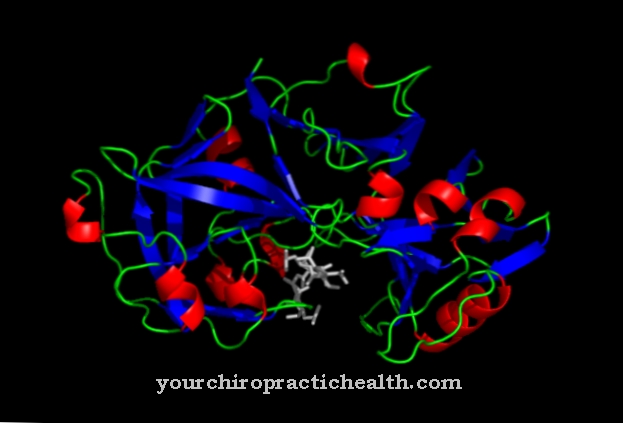
The C-reactive protein (CRP) is part of the immune system and mediates unspecific immune reactions. It can serve as a marker for inflammatory processes in the organism, whereby the focus of inflammation cannot be specified and localized. CRP is one of the so-called acute phase proteins.
What is a C-reactive protein?
The C-reactive protein always occurs in increased concentrations in the organism during inflammatory reactions. It is an acute phase protein that is formed immediately in the event of an infection or injury to support the immune system.
Elevated CRP values can be measured even before the actual inflammation starts. As soon as the inflammation subsides, the CRP concentration immediately falls back to the normal value. CRP is a so-called opsonin that stimulates the complement system. As opsonin, it identifies antigens such as bacteria and fungi or the body's own cells with destroyed cell membranes for attack by macrophages (scavenger cells). An opsonin is a bridging molecule which makes bacterial and dead cell substance recognizable for the phagocytes by docking.
As part of the complement system, protein complexes are formed from parts of the antigen with CRP or antibodies. These protein complexes act as docking points for the phagocytes. The C-reactive protein consists of 206 amino acids and belongs to the family of pentraxins. Pentraxins are composed of five identical protomers. It is produced when needed in the liver as a result of stimulation by interleukin-6 (II-6).
Function, effect & tasks
The C-reactive protein is part of the immune system and plays an important role in preparing for an immune response. It serves as a non-specific indicator of inflammatory reactions in the body. The normal concentration of CRP in the organism is usually below 10 milligrams per liter.
If increased concentrations are detected in the organism, an inflammatory reaction takes place somewhere in the body. It reacts particularly strongly to bacterial infections, rheumatic diseases, other autoimmune reactions in the body or severe necrosis in the case of injuries or serious pathological processes. In the course of these processes, a lot of dead organic material is created, which has to be broken down by macrophages. The CRP concentration also rises with virus infections. But here the increase is nowhere near as strong. CRP works by binding to the phospholipids on the cell membrane. This includes the cell membrane of bacteria, fungi and dead body's own cells, which form a protein complex with CRP.
This protein complex is now taken up by the macrophages and broken down further. This reaction can be compared to garbage disposal. Virus infections are rarely displayed because viruses do not have a cell membrane and penetrate the cell to multiply. Only when the host cell is destroyed do C-reactive proteins form, which attach to the destroyed cell membrane.
Education, occurrence, properties & optimal values
The non-specific immune response of CRP is much faster than the specific response of the immune system. The determination of the parameters can therefore give a quick overview of whether an inflammatory reaction is present. The values are already significantly increased before the white blood cell count rises and fever occurs if diseases such as appendicitis, respiratory tract infections, intestinal infections or urinary tract infections are suspected.
In children, even harmless infections can lead to a sharp rise in values. The CRP level decreases in line with the inflammation within the body. In contrast, the blood sedimentation does not normalize until later. Acute and chronic inflammatory processes can be clearly distinguished. In acute inflammation, the CRP values rise more strongly than in chronic processes. The CRP values also provide good information if there is a suspicion of rheumatic processes. Furthermore, the measurement is also used to record complicated infections that can occur after operations or problems during pregnancy.
The examination can also provide clues as to the distinction between viral and bacterial infections, since the values do not increase as much in viral infections. However, determining the CRP values alone is not sufficient here. Finally, the CRP measurements also provide early indications of the success of an anti-inflammatory or antibiotic treatment. The decrease in inflammatory processes or the bacterial load correlates with the decrease in CRP values.
Diseases & Disorders
The severity of the disease also correlates with the measured CRP values. As already mentioned, the normal concentration of C-reactive protein in the body is below 10 milligrams per liter. With values between 10 and 50 milligrams per liter, there is usually slight and local inflammation. Slightly increased CRP values are also possible in smokers and competitive athletes.
Concentrations above 50 milligrams per liter already indicate severe inflammation.At a concentration of over 100 milligrams per liter, the most severe infectious processes, severe autoimmune diseases or even tumors are to be expected. With the constant measurement of the CRP values during the disease process, the course of the respective disease can be well documented. This also applies to monitoring the course of immune reactions after an organ transplant. When the body reacts to rejection, the CRP values naturally also rise. In the case of known chronic diseases that arise on the basis of autoimmunological processes such as Krohn's disease or rheumatic diseases, the current inflammatory status can thus be easily determined.
In the event of a disease flare-up, the values are of course much higher than in an inactive intermediate phase. Persistent high levels of inflammation can indicate the risk of later arteriosclerosis, diabetes mellitus and metabolic syndrome. Although the course of a diagnosed infection, autoimmune disease or the rejection reactions in an organ transplant can be followed by measuring the CRP values, a primary diagnosis of the present disease is not possible through this examination.