Candida dubliniensis is a yeast and is often found in the oral cavity of HIV and AIDS patients. In addition, it often occurs together with Candida albicans in candidiasis. The similarity between Candida dubliniensis and Candida albicans makes it difficult to correctly identify the microorganism.
What is Candida Dubliniensis?
In 1995, scientists differentiated Candida dubliniensis from the very similar fungus Candida albicans.In the context of candidiasis, Candida dubliniensis often occurs together with Candida albicans or other species of this genus.
The species name “dubliniensis” goes back to the Irish capital Dublin, as researchers recognized the yeast in this part of Europe as a new species for the first time. Within this classification, different types of Candida dubliniensis can be distinguished, one of which may have pathogenic properties. However, since the fungus occurs almost exclusively with other Candida species, it is difficult for experts to assess its general importance for medical practice.
Occurrence, Distribution & Properties
Although Candida dubliniensis was not described until the 1990s, examinations showed the microorganism retrospectively for a period of at least 40 years. Presumably, Candida dubliniensis is therefore not a new species or mutation. Instead, researchers assume that it has often been confused with Candida albicans in the past.
The microorganism is distributed worldwide. In 1998, scientists Sullivan and Coleman found that the frequency of the different types of Candida was shifting. The number of infections with Candida albicans is falling proportionally, while other types are gradually taking their place. However, Candida albicans is still the most common cause of Candida infections.
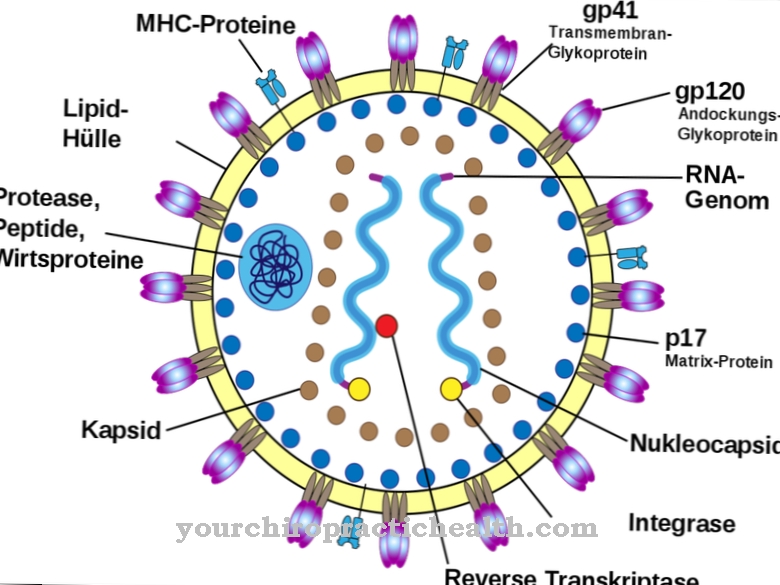
Oral mucosal swabs from people with HIV or AIDS contain spores of Candida dubliniensis more than the average. However, candidiasis does not necessarily break out, as a strong immune system provides natural protection against pathogens. Since it is precisely this defense system that is weakened in people with AIDS (or other significant infections), the fungus is able to spread.
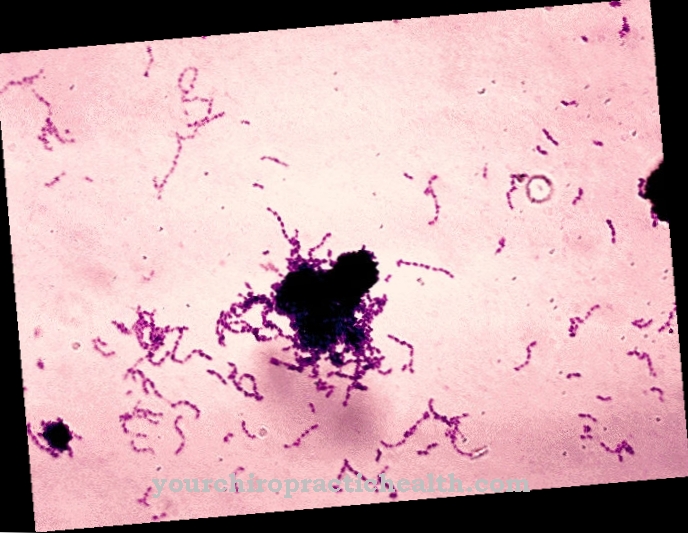
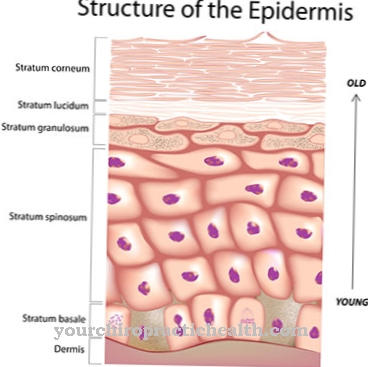
When viewed with the naked eye, Candida dubliniensis forms a whitish coating on infected surfaces. At first it often forms a flat settlement, but especially after a longer period the fungus can form into small colonies that are separated from each other.
The microorganism forms chlamydospores and tubes similar to them in some cases, but not constantly. Chlamydospores are capsules or vesicles that form on branches of the fungal plexus and initially remain in contact with the rest of the organism. The bladder consists of the cell wall, which thickens and thus forms a resistant protective layer. If the environment dries out or does not provide enough nutrients, the organism can survive in these shells. The surrounding tissue dies, but the fungus can grow again from the retreat in the chlamydospore. For medicine, this can mean more difficult treatment, since the organism can be temporarily inactive, but still present.
The fungus reproduces optimally at 30–37 ° C, but not at over 42 ° C. Laboratories take advantage of the maximum temperature of growth by creating cultures with spores and allowing them to rest at 42 ° C for 48 hours. If the spores are Candida dubliniensis, no coating will grow on the prepared nutrient medium. If, on the other hand, it is the very similar Candida albicans, the fungus multiplies and a characteristic whitish layer develops.
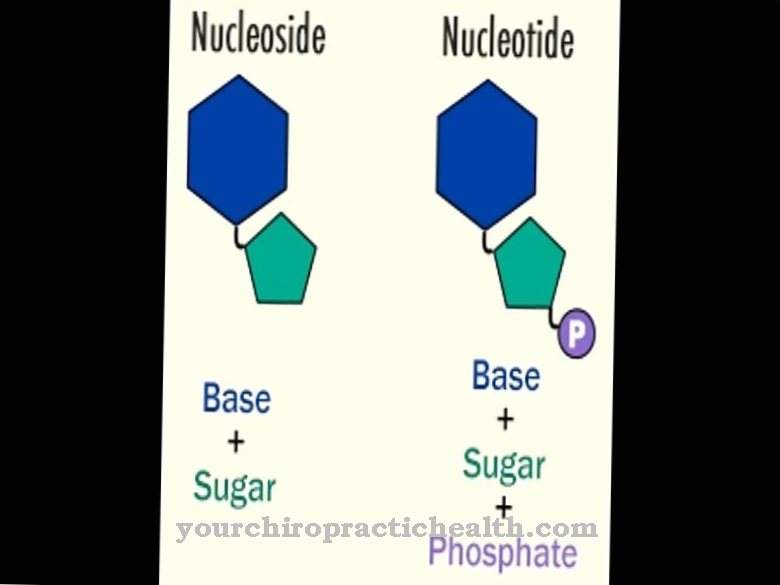
In this way, the distinction between the two microorganisms succeeds. In addition, Candida dubliniensis and Candida albicans develop different colorations on special culture media. The two microorganisms also differ in terms of their genetic make-up. Candida dubliniensis usually has a diploid set of chromosomes in which each chromosome appears twice, but the fungus can temporarily take on a haploid form.
Illnesses & ailments
Candida dubliniensis is particularly common in the oral cavity of patients who are infected with the HI virus or who suffer from AIDS. The latter describes a specific syndrome that disrupts the human immune system as a result of an HIV infection and progressively decomposes it, while the infection with the HI virus in itself can (initially) be symptom-free.
Candida dubliniensis is also involved in the formation of candidiasis in many cases. Symptoms include white coating in the mouth (for example, on the tongue or in the esophagus), on fingernails, or in folds of skin. In the case of systemic candidiasis, Candida dubliniensis can affect numerous organs.
The disease mainly occurs in people whose immune systems are not fully functional. The possible cause can also be the temporary use of antibiotics, cancer and associated medication, diabetes mellitus, sepsis or another underlying disease. Candida dubliniensis has so far played a minor role in candidiasis.
Various antifungal agents are used in the treatment of the infectious disease. This group of drugs fights the microorganisms and prevents their further spread in the tissue.
"Candidiasis as a result of HIV disease" is an independent diagnosis in the international classification system of diseases (ICD) (B20.4). The fungal infection often manifests itself in those affected as one of the first visible signs of an increasingly weakened immune system. In addition, an investigation was able to prove the colonization with Candida dubliniensis in the lungs of a deceased person in a single case. It is not known whether the infection contributed to the death or was accidental.




.jpg)









.jpg)

