At Cefmenoxime it is a synthetic antibiotic that belongs to the group of cephalosporins. It develops its strong bactericidal effect by inhibiting the cell wall synthesis of the infectious bacteria. The classic pathogens that are treated with cefmenoxime include: a. Staphylococci, Streptococci and E. coli bacteria.
What is cefmenoxime?
Cefmenoxime is a synthetic antibiotic that has a strong bactericidal effect. This means that it kills infectious bacteria in a targeted and efficient manner. The medicinal substance owes its effectiveness to the inhibition of the cell wall synthesis of the infectious bacteria. It is no longer possible for them to keep themselves alive. They die.
Because of this mode of action, it is assigned to the third generation of the group of so-called cephalosporins, which also includes the antibiotics ceftriaxone, cefotaxime and cefuroxime.
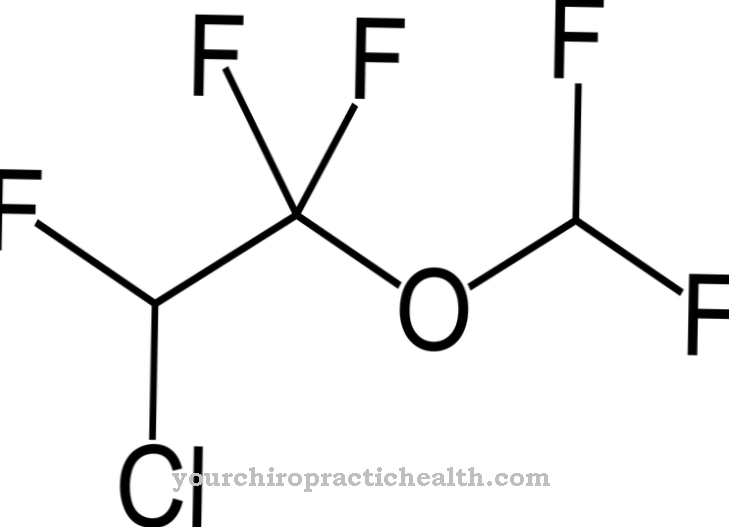
In the medical and pharmacological literature, cefmenoxime belongs to group 3a of the cephalosporins. These are known as beta-lactam antibiotics. The white to yellowish-white fabric is sold under the trade name Tacef®. In chemistry and pharmacology, the substance is described by the chemical formula C 16 - H 17 - N 5 - O 7 - S 2, which corresponds to a moral mass of 455.47 g / mol.
Pharmacological effect
Cefmenoxime belongs to the third generation of the beta-lactam antibiotic class of active substances (group 3a according to the Paul Ehrlich Institute classification). As such, it has a four-membered lactam ring and goes back to the original form of penicillin. The effect of cefmenoxime is therefore bactericidal. Infectious bacteria are thus specifically killed.
Cefmenoxime does this by inhibiting peptidoglycans (molecules made up of sugars and amino acids in the bacterial cell wall). These play a major role in bacterial cell division and are therefore vital. After the inhibition process triggered by cefmenoxime, the bacteria die.
85% of cefmenoxime is excreted renally (through the kidneys). The half-life of the drug is - which is typical for representatives of his group - about 70 minutes.
A good pharmacokinetic distribution to bone, wound secretion, urine and skin could be determined. The distribution between liquor and bronchial secretions, however, is only moderate. Furthermore, there are already some cross-resistances with cefotiam, cefuroxime, cefamandol and cefazolin.
Medical application & use
Cefmenoxime is prescribed in human medicine to treat severe infections. These include sepsis, pneumonia (lung infections), wound infections, meningitis, osteomyelitis and inflammation of the bile. However, there is also an indication for infections that are associated with a serious underlying disease (e.g. neuroborreliosis).
The spectrum of antibacterial activity of cefmenoxime includes numerous gram-positive and some gram-negative bacteria. A bacterium is considered gram negative if it turns red when differential staining is performed. If it turns out to be blue, then it is considered gram-positive.
In particular, staphylococci, Haemophilus influenzae, Salmonella, Shigella, Morganella and Serratia can be combated well with cefmenoxime.
Cefmenoxime has been approved for the treatment of adults and children as well as adolescents. The usual dose for a healthy adult is max. 4 times 3 g. For children, 50-200 mg per kilogram of body weight is usually prescribed. Since most of the drug is broken down renally, the dosage should be reduced in the case of severe kidney dysfunction.
Risks & side effects
Cefmenoxime can lead to undesirable side effects. Allergic reactions are also possible. Before using it for the first time, it must therefore be checked whether there is an allergy or intolerance to cefmenoxime or other representatives of group 3a of the active ingredient class of cephalosoporins. In these cases there is a contraindication.
Incompatibilities can manifest themselves in the form of a high fever or extreme skin reactions (reddening, itching, heating, etc.).The treatment must then be suspended and medical advice sought immediately.
The undesirable side effects that can occur as part of therapy also include increased bleeding tendencies, alcohol intolerance, positive Coombs tests and an increase in transaminase values.