Tigecycline is an antibiotic that is produced semi-synthetically. It is used for complicated infections and for infections with multi-resistant problem strains.
What is tigecycline?

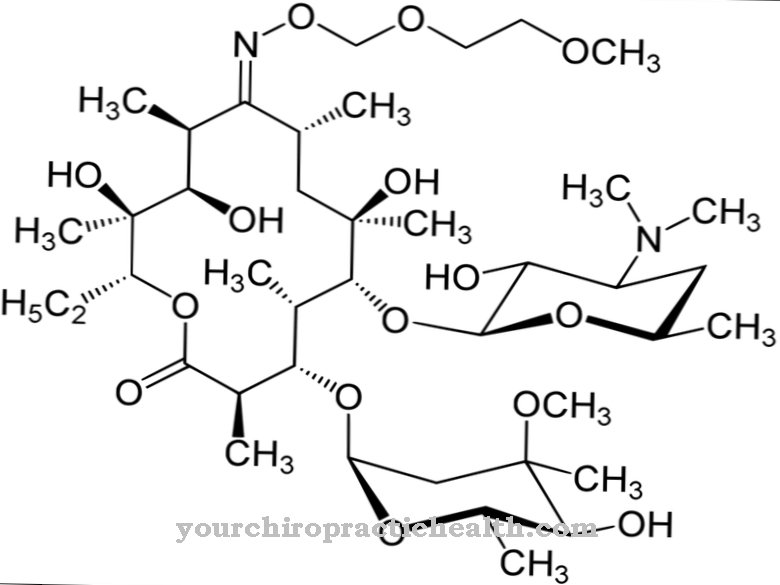
The drug tigecycline is one of the tetracycline antibiotics and one of the antibiotic drugs from the class of glycylcyclines. Tigecycline is a derivative of the tetracycline. Since the drug acts against many different pathogens, it is used as a broad-spectrum antibiotic. Broad spectrum antibiotics capture many bacteria from the gram negative and gram positive range. They also work against chlamydia, rickettsiae, spirochetes and protozoa.
Tigecycline also works against anaerobes such as clostridia. Infections caused by Escherichia coli or Acinetobacter baumannii can also be treated with tigecycline. Tigecycline is currently also effective against methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VCE) and against ESBL-producing pathogens. Since tigecycline has to be used more and more frequently due to increasing resistance, further resistances can be expected in the future due to the widespread use of the antibiotic.
Pharmacological effect
Tigecycline works like most tetracyclines. The drug inhibits protein synthesis on the ribosomes of the pathogen. As a result, aminoacyl-tRNA can no longer accumulate on the 30S subunits of the ribosomes, so that the bacteria can no longer multiply.
In contrast to other tetracyclines, tigecycline can bypass two mechanisms of resistance. Many resistant bacteria have so-called efflux pumps. These remove the antibiotic from the bacterial cell using transport proteins. Tigecycline can circumvent this protective mechanism. In addition, it has a five-fold higher binding affinity to the ribosomes, so that various protective proteins of the bacteria become ineffective.
Medical application & use
Tigecycline is a reserve antibiotic. Reserve antibiotics are special antibiotics that are used exclusively to treat infections with resistant pathogens. In the case of severe infections, they can also be used as calculated antibiotic therapy. They are administered immediately if the pathogen is still unknown in the case of a severe infection, but can be recognized due to the symptoms. By starting therapy quickly, complications should be prevented.
In Germany, tigecycline is only approved for the treatment of severe infections. The drug is administered intravenously. A possible area of application is severe skin and soft tissue infections and complicated infections within the abdomen. In most cases, these complicated infections are acquired on an outpatient basis and caused by MRSA (meticillin-resistant Staphylococcus aureus).
Infections with ESBL-producing pathogens are also an indication for tigecycline. ESBL stands for Extended Spectrum Beta-lactamases. ESBL-forming bacteria can break down antibiotics containing beta-lactam and are therefore resistant to penicillins, cephalosporins and monobactams. ESBL-forming bacteria belong to the so-called problem germs. They are responsible for a wide variety of infections in hospitals. ESBL-forming Klebsiella or Escherichia coli are particularly important. So far, tigecycline is still effective against these pathogens. The antibiotic, however, cannot do anything against infections with Pseudomonas aeruginosa.
Risks & side effects
There are still no studies on the effectiveness and side effects of tigecycline for children and adolescents under 18 years of age. However, there is already evidence that tigecycline can disrupt bone formation in children and adolescents, so that bone formation can be delayed.
The side effect of tigecycline depends on the dose. It is therefore recommended to split the daily dose into two individual doses. Common side effects are nausea and vomiting. In comparison with other antibiotics, an increased mortality was found. In pneumonia in particular, treatment with tigecycline is associated with a higher mortality rate. The course of the disease is particularly negatively influenced if a superinfection occurs during treatment with tigecycline. A superinfection is a bacterial infection that develops from a viral infection. Due to the high mortality, a thorough risk-benefit assessment should be carried out before using tigecycline. If, after starting therapy, it turns out that the infection is not part of the approved indications, alternative antibacterial treatment should be carried out.
In contrast to many other antibiotics, tigecycline is not metabolized via the so-called cytochrome P450 system. Therefore, there is little interaction between the antibiotic and other drugs. If the anticoagulant warfarin is administered at the same time, the coagulation parameters in the blood must be checked.
It should be noted that oral contraceptives may not work effectively while taking tigecycline.










.jpg)

.jpg)
.jpg)











.jpg)