As Chemosynoviorthesis is a procedure in the context of the therapy of arthritic changes in the synovium (synovial membrane, synovial membrane) in inflammatory joint diseases. Analogous to the radiosynoviorthesis (injection of radioactive substances), a chemical drug is injected into the affected joint to sclerotise the synovial membrane.
What is the chemosynoviorthesis?

A Chemosynoviorthesis is a therapy method for rheumatic or arthritic joint diseases such as rheumatoid arthritis (also rheumatism). For this purpose, a chemical drug (including osmic acid, sodium morrhuate) is injected into the affected joint to destroy the pathologically altered synovium.
By sclerotherapy of the synovial membrane, a renewal and reconstruction of the affected synovial membrane should be stimulated. The treatment process often leads to a long-term improvement in swelling, pain and the function of the treated joint.
In the case of larger joints in particular (including the knee joint), chemosynoviorthesis is often performed following surgical removal of the synovial membrane (synovectomy) in order to obliterate the remaining synovial remnants in the joint.
Function, effect & goals
A Chemosynoviorthesis is mainly used for recurrent or chronic inflammation of the synovial membrane (including rheumatoid arthritis, rheumatoid arthritis), which is accompanied by painful joint swelling.
Particularly in the case of monarthritic processes in which a single joint is affected, a chemosynoviorthesis is used to try to switch off the soil or the pathologically changed tissue structures on which the arthritis can develop locally with a chemical drug, so that a healthy synovium can subsequently be formed can develop in the affected joint. A chemosynoviorthesis can also be indicated if there is no indication for joint surgery or synovectomy or other surgical procedures are contraindicated.
A chemosynoviorthesis is also used in the presence of active mono- or oligoarthritis (a few joints are affected) as well as chronic polyarthritis with synovitis (inflammation of the joint lining) of individual, especially smaller joints. Chemically induced sclerotherapy can also be indicated in the case of recurrent synovitis as a result of surgical synovectomy. In the run-up to chemosynoviorthesis, an X-ray image of the joint to be treated should be made in order to be able to exclude pronounced signs of destruction, exposed joint bodies and aseptic bone necrosis.
In addition, joint effusions should be localized using a sonogram (ultrasound image) and delimited from proliferating (overgrown) tissue structures. Following the disinfecting measures, any existing joint effusions are first punctured. To rule out a periarticular injection, a diagnostic injection with a local anesthetic (including scandicain) should then be carried out before the sclerosing drug is injected intraarticularly.
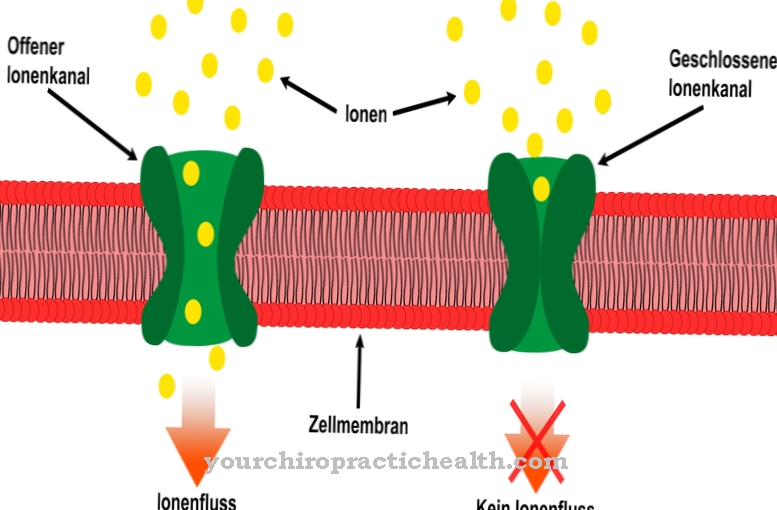
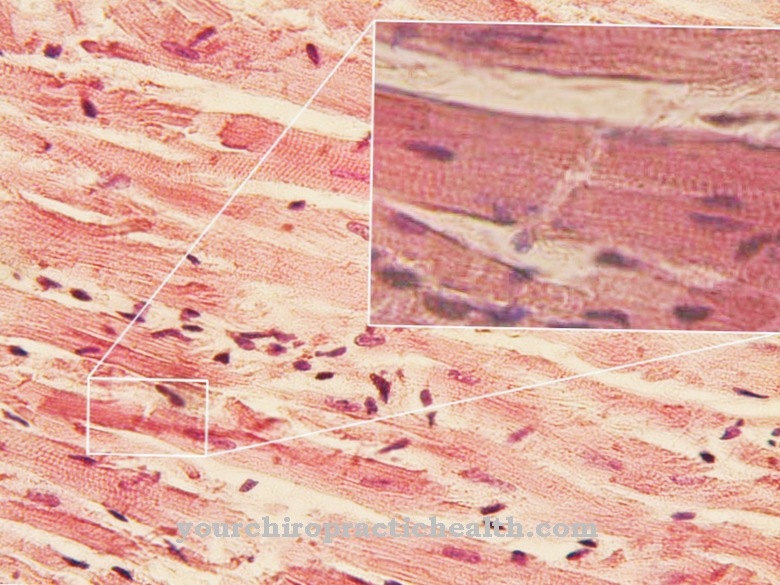
The most common substances used in chemosynoviorthesis are osmic acid and sodium morrhuate. Osmic acid is absorbed by the synovial cells and causes coagulation necrosis in the treated tissue structures. After intra-articular injection, sodium morrhuate causes cytolysis (cell dissolution) through damage to the cell membrane, which is locally associated with a massive inflammatory reaction and synovial membrane necrosis.
In addition, immune-competent tissue structures such as pathologically changed T cells, which are responsible for rheumatic inflammation, among other things, are destroyed by the inflammatory reaction. For the 48 hours following the chemosynoviorthesis, the affected joint should be immobilized and adequately cooled (e.g. with ice packs). In some cases, the chemosynoviorthesis is repeated one or more times.
Risks, side effects & dangers
Common side effects following a Chemosynoviorthesis are swellings, redness and pain in the area of the affected joint (worsening of the findings), which are induced by the breakdown of the sclerosed mucous membrane and the corresponding inflammatory processes and are treated as part of symptomatic therapy (including cooling, anti-inflammatory and pain-relieving drugs).
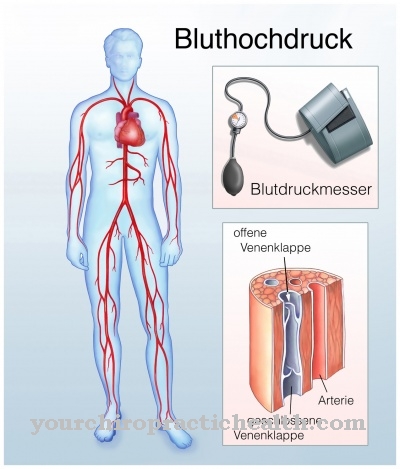
Serious side effects or complications are rarely observed with chemosynoviorthesis. However, the spread of pathogens on the skin into the interior of the joint can have dangerous consequences. In extremely rare cases, swelling of soft tissues near the treated joint, which can lead to thrombosis, may be noticed. Systemically, i.e. related to the entire human organism, temporary fever and increased liver and blood cell values can occur.
In addition, unintentional injection of the sclerosing medication into soft tissue structures can cause pain and local inflammation, which, however, usually have no consequences. Chemosynoviorthesis is also contraindicated in the presence of pregnancy and in the presence of liver and / or kidney insufficiency. On the patient side, attention should be paid to consistently following the physiotherapy and the symptom-dependent build-up of stress in order to avoid drug-induced capsule shrinkage after chemosynoviorthesis. Damage to the articular cartilage can usually be ruled out with a chemosynoviorthesis.