Condylomata acuminata are considered a sexually transmitted disease that is caused by an infection with papillomavirus and manifests itself as nodular skin growths. Across Europe, around 1 to 2 percent of the sexually active population is affected by Condylomata acuminata, with the peak between the ages of 20 and 24.
What is condylomata acuminata?

© Kyrylenko - stock.adobe.com
Condylomata acuminata (also genital warts, condylomas) are benign (benign) nodular growths of the skin the size of the head of a pin, which are caused by an infection with human papillomaviruses (HPV) and which usually affect the anogenital area.
In most cases, the infection does not cause any symptoms besides the wrinkled, red-brownish or gray-whitish skin growths that can lead to pruritus (itching), discharge or burning sensation. In contrast, the psychological stress and impairment of sexual life are to be assessed as much greater.
Women are mostly affected in the area of the vaginal entrance, the cervix (cervix uteri) and less often the urethral orifice, while men primarily have condylomata acuminata on the glans penis (glans), foreskin, anus, urethral orifice and rectum.
causes
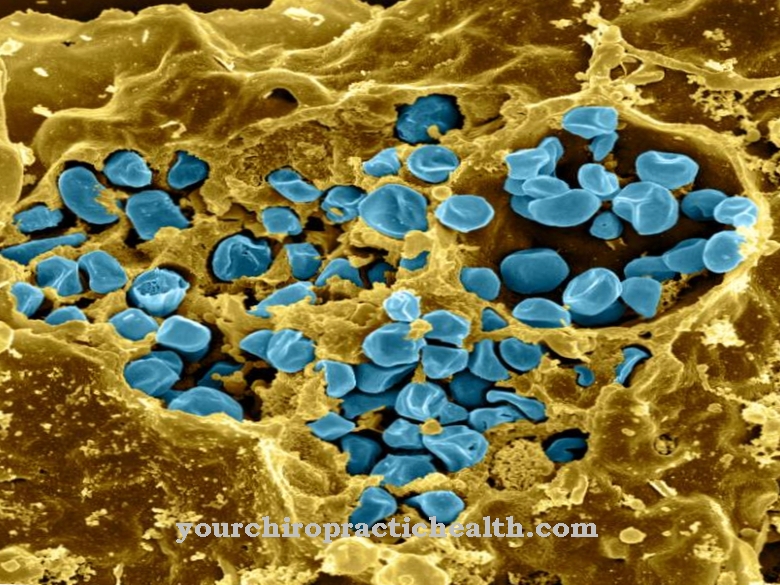
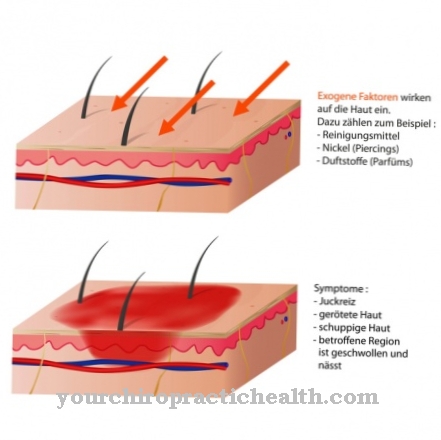
Condylomata acuminata is caused by human papillomaviruses (HPV), in particular by sero types 6 and 11, in rare cases also by types 16 and / or 18, which are usually caused by unprotected sexual contact or a smear infection (including via contaminated sex toys) are transferred to the skin.
Here, the viruses first colonize the upper layers of the skin, into which they get through small lesions in the skin or mucous membrane of the anus, rectum, vagina or penis. If the immune system is weakened as a result of HIV, immunosuppressive medication or drug abuse, these can multiply and cause tissue growth with warts.
Fungal infections, genital herpes or eczema also promote infection. In addition, an infected mother can infect her newborn child with papillomaviruses during birth and cause condylomata acuminata.
Symptoms, ailments & signs
Condylomate acuminate are benign skin growths. They can be recognized by their typical shape, which is reminiscent of normal warts. Genital warts reach the size of the head of a pin, and occasionally they get larger. They are reddish to brownish or gray-white in color and usually occur in several groups that are close together.
These wart beds typically cause severe itching, combined with tenderness and possibly bleeding. They usually occur in the genital area or on the feet. In women, they usually grow on the labia, at the entrance to the vagina, in the cervix or in the mouth of the urethra. In men, they mainly develop on the foreskin, glans, anus, urethral entrance and rectum.
In the absence of treatment, genital warts can spread to other parts of the body. If genital warts are opened, a purulent secretion flows off, which usually smells unpleasant. Condylomas can be accompanied by a feeling of illness. Some sufferers complain of fever, nausea and vomiting and other symptoms, which always depend on the underlying disease.
Genital warts are usually associated with psychological complaints. The skin growths create a cosmetic blemish. Those affected are often ashamed of it and withdraw from social life. Serious emotional problems such as fears, inferiority complexes, feelings of guilt or depression can develop over time.
Diagnosis & course
As a rule, Condylomata acuminata can be diagnosed on the basis of the skin condition or the characteristic wart formation in the anogenital area. With the help of the so-called acetic acid test, the affected areas can be localized as white discolored areas.
An HPV-DNA test and a PCR (polymerase chain reaction) allow the detection of the specific papilloma virus. The diagnosis is confirmed by means of a biopsy with subsequent histological analysis. An intra-anal or intrarectal infection can be excluded by an endoscopic examination.
In the differential diagnosis, the disease should be differentiated from fibroids and squamous cell carcinoma of the genital area as well as from precancerous diseases and certain forms of hirsuties. Condylomata acuminata usually show a good course with a very good prognosis, although recurrences are not uncommon. The risk of cervical cancer is estimated to be low for the HPV types, which mainly cause condylomata acuminata.
Complications
In most cases, the condylomata acuminata lead to the so-called genital warts on the genital organs. These are strong growths that are associated with relatively strong and burning pain and thus extremely reduce the patient's quality of life. The sexual organs also experience severe itching, which is associated with reddening.
The complaints reduce sexual desire enormously, which can also lead to depressive moods and other psychological complaints. Because the symptoms are relatively characteristic, the disease can be diagnosed early so that treatment can also be started early. The treatment itself is symptomatic and primarily alleviates the symptoms.
Creams, ointments and medication are used, with no further complications. The growths can be removed with the help of surgical interventions. However, this does not prevent a new illness. Complications, as a rule, can only arise if the disease is left untreated and spreads to neighboring regions. With early treatment, the disease always progresses positively.
When should you go to the doctor?
A doctor does not necessarily have to be consulted with Condylomate acuminata. Most genital warts do not cause any discomfort and will peel off on their own after a while. However, if the growths bleed, oozed, severely itched or caused other complaints, medical advice is required. Warts that enlarge or multiply quickly are also best examined by a specialist and treated if necessary. Genital warts that appear or keep coming back for no apparent reason indicate a serious illness - in this case it is essential to speak to your doctor.
Children and the elderly should always see a doctor with Condylomate acuminata in order to rule out serious illnesses and complications. The same applies to patients with neurodermatitis or other skin diseases. If you have already been infected with HP viruses, it is best to consult a general practitioner if it occurs again. Other contact persons are the dermatologist, urologist or gynecologist. If the Condylomate acuminata have a strong influence on well-being and represent an emotional burden, you should speak to a therapist.
Doctors & therapists in your area
Treatment & Therapy
The therapeutic measures for condylomata acuminata primarily depend on the extent of the infection and the location. If the outer layers of the skin are affected, solutions or ointments or creams with podophyllotoxin (cytostatic agent), silver nitrate, epigallocatechin gallate, which is contained in green tea, or imiquimod, a virostatic agent that stimulates the body's immune system, are recommended for topical application over several weeks .
Podophyllotoxin, which inhibits cell division, should not be used during pregnancy. If there are internal infections in the mucous membranes of the vagina, anal canal or in the area of the urethral orifice, treatment with trichloroacetic acid, which is applied to the affected areas at weekly intervals, may be indicated.
In addition, the skin growths can be frozen by cryotherapy using liquid nitrogen. In both cases, a local anesthetic can be applied due to the accompanying pain. In the case of bed-like or pronounced growths as well as recurrences, surgical intervention may be considered. The genital warts are removed either with the help of a curette (including a sharp spoon) or as part of an electrocautery (heat-generating electric current) or laser therapy under local or general anesthesia.
Photodynamic therapy (PDT) using 5-aminolevulinic acid can also be used if appropriate. In the case of repeated relapses, therapy with gels containing interferon-beta may be indicated in order to prevent a renewed manifestation of condylomata acuminata.
Outlook & forecast
The prospect of a cure for condylomata acuminata depends on the time of diagnosis and the start of treatment. There is no spontaneous healing and alternative healing methods are ineffective. The prospect of recovery can only be achieved through medical treatment. With early medical care, a good prognosis is possible.
The skin abnormalities are removed in a surgical procedure and a subsequent treatment to get rid of the human papillomavirus (HPV) is initiated. If the outcome is favorable, the patient can be discharged as symptom-free within a few weeks. For permanent healing, protection against reinfection of the HPV is necessary.
If the growths have already spread, the risk of a malignant course of the disease increases. The genital warts can lead to the formation of metastases. There is a possibility that cancer cells will peel off and spread to the body through the bloodstream. In severe cases, organs or other regions of the body become cancerous. For the patient, this situation represents a potential danger to life.
The condylomata acuminata has a high rate of recurrence. People who have the HPV are at high risk of genital warts coming back. Sick people in whom the condylomata acuminata was very pronounced also show a higher susceptibility to recurrence than other patients.
prevention
An infection with HP viruses and accordingly also condylomata acuminata can be prevented by protected sexual intercourse or the use of condoms as well as by a prophylactic vaccination against HP viruses. In addition, direct contact with infected skin areas should be avoided. As a rule, the partners of those affected should also be examined for condylomata acuminata in order to rule out a ping-pong infection (mutual re-infection).
Aftercare
When condylomata acuminata occurs, there is only extremely rare or almost never complete healing. On the contrary, degeneration of the condylomata is possible in the long term. In many cases, the condylomas become malignant. That worsens the prognosis. For this reason, close and sufficiently frequent follow-up care for the affected patient is essential.
After surgery or an ointment treatment, the follow-up examinations are initially carried out at intervals of three to four weeks. Later, the intervals between individual follow-up examinations can be increased. With professional treatment and sensible therapy, the chances of recovery are quite good. The problem, however, is that even surgical removal of the genital warts does not guarantee 100% security against recurrence. The reason for this lies in the viral causation of the condylomata acuminata. Only their visible consequences can be removed.
During postoperative follow-up care, it is often discovered that there is again a minor infestation of genital warts. Since it cannot make sense to proceed surgically for every relapse, therapy with antiviral ointments or solutions is advisable in this case. However, if necessary, immediate surgical intervention is required in the case of condylomata acuminata. The point of close follow-up care is to prevent severe courses. The involvement of papilloma vaviruses carries the risk of degeneration and a high risk of infection.
You can do that yourself
Genital warts in the genital area are extremely uncomfortable and stressful, but generally not dangerous. Nevertheless, you should definitely refrain from purely self-treatment and consult a doctor immediately.
The human papillomaviruses (HPV) that cause the infection are highly contagious and are predominantly transmitted during sexual intercourse, even if other routes of transmission cannot be ruled out. The best self-help measure is to avoid the contagion. The viruses penetrate the organism through tiny skin injuries.
Certain sexual practices, which are increasingly associated with minor injuries to the mucous membranes, as is the case in particular with anal intercourse, are therefore particularly risky. Therefore condoms should be used during sexual intercourse. These do not guarantee 100% protection, as touching infected parts of the body can be enough to become infected. However, condoms significantly reduce the risk of infection.
Anyone who is affected by an acute genital warts infestation must never have sexual intercourse. In this situation there must not be any hygiene deficits, otherwise a smear infection threatens. In particular, towels and items of clothing that lie next to the skin should not be shared. Laundry and other items of clothing that have come into contact with infected parts of the body should be washed at at least 60 degrees.
Strengthening the immune system through a healthy, vitamin-rich diet can also help to overcome an infection more quickly or to prevent the disease from breaking out in the first place.

.jpg)
.jpg)













.jpg)