When the intestine stands still, nothing works in the digestive tract - severe pain, infections and other complications can occur within a very short time. A Intestinal paralysis or Intestinal atony must therefore be recognized, monitored and quickly rectified. Below is a brief overview of the possible causes.
What is intestinal paralysis?
An intestinal atony is the loss of tone in the intestine, i.e. a loss of muscular tension in the intestinal wall and thus, simply put, intestinal paralysis. This prevents the further transport of food, thus leads to constipation and intestinal obstruction and a whole series of other complications.
causes
There are several causes of intestinal atony. A fundamental distinction is made between circulatory disorders and reflex-like bowel arrests - in both cases, however, the impairment of the nervous system is "to blame" for the arrest of the bowel wall.
Circulatory disorders of the intestinal wall are primarily a problem of older people, whose blood vessels are altogether changed by arteriosclerosis in such a way that less blood passes through them. If the blood vessels in the intestine are narrowed, abdominal pain (angina abdominalis) occurs, especially after eating, because a lot of blood is then required in the intestine and the supply bottleneck is particularly significant.
This can permanently lead to chronic damage to the intestinal wall, acute mesenteric infarcts can form due to sudden detachment of the thrombus, embolisms and vascular occlusions (analogous to myocardial infarction). The intestinal section then no longer receives any blood and the cells quickly die - so there is no longer any movement in the intestinal wall.
Circulatory disorders can also occur in regionally limited areas if the intestinal wall is "crushed" from the inside by a tumor, a mechanical intestinal obstruction or a stuck foreign body and blood flow is no longer possible.
The other major group of causes of intestinal paralysis are the intestinal protective reflexes, which can occur in a number of disease processes in the abdominal cavity or in the space behind the peritoneum. Here, too, an intestinal obstruction can play a role, which reflexively ensures that the upstream part of the intestinal tube no longer pushes the food on.
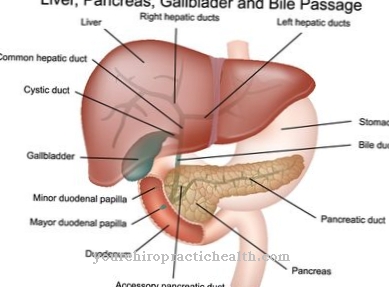
Even massive inflammations paralyze the intestinal wall via this mechanism, e.g. large peritonitis. In addition, diseases of other organs such as inflammation of the pancreas (pancreatitis) or kidney stones can irritate the area and thus also affect the nerves that pull past these organs towards the intestinal wall. A so-called "paralytic ileus" (intestinal obstruction due to paralysis) is therefore often an accompanying symptom of these diseases.
Congenital causes such as Hirschsprung's disease, in which nerve plexuses are simply missing in the lower sections of the intestine, can lead to intestinal atony and related problems in the first few years of life. Finally, modern medicine can also be the cause of intestinal atony: In addition to some drugs (opiates), major surgical interventions in the abdominal cavity can reflexively paralyze bowel activity hours to days after the operation.
Symptoms, ailments & signs
.jpg)
© decade3d - stock.adobe.com
Intestinal paralysis leads to various gastrointestinal complaints. Typically, constipation or stool retention occurs, accompanied by abdominal pain, nausea and vomiting, as well as a bloated stomach. The symptoms mainly occur after eating and usually persist for a few minutes to hours before they slowly subside.
Also in the morning after getting up and late in the evening there is increased stomach pain and flatulence. If the intestinal atony remains untreated for a longer period of time, further complaints can arise. In the worst case, the constipation develops into a complete intestinal obstruction. An ileus is always associated with extreme pain and cramps in the abdomen.
An intestinal obstruction can also be recognized by the blood in the stool, blood often leaks from the anus. An intestinal obstruction can damage the intestinal wall and cause peritonitis. If the course is severe, an ileus leads to death.
Postoperative intestinal paralysis is associated with an increased risk of infections, as the hospital stay is considerably longer. It can also lead to wound healing disorders, infections and other complications in the surgical area. Outwardly, intestinal paralysis is usually not visible. Only the disturbed bowel movement indicates a disease that needs to be clarified and treated.
Diagnosis & course
The reduced gastrointestinal passage due to the paralysis of the intestinal wall sooner or later leads to a paralytic ileus, i.e. a complete intestinal obstruction.
First of all, this means that nothing comes out below. By the time the affected person notices this, however, other, more serious symptoms usually occur. In particular due to the inflammation or the lack of oxygen, which are often the basis of intestinal atony, massive abdominal pain usually occurs. When the intestinal wall dies, blood in the stool or major intestinal bleeding can also occur. Kidney stones lead to cramp-like pain, pancreatitis causes massive belt-shaped pain in the upper abdomen.
A serious complication of a paralytic ileus is the migration of intestinal bacteria through the intestinal wall - if these enter the abdominal cavity and inflame the peritoneum (peritonitis), it is always life-threatening.
The diagnosis is based on anamnesis (typical abdominal pain after eating, atrial fibrillation as a source of embolism, alcohol consumption as an indication of pancreatitis, etc.) and physical examination (abdominal tension as a protective reflex, intestinal noises present?, Blood on the finger cot during the rectal examination, etc.).
An X-ray (abdomen overview) may show stagnant intestinal loops and fluid levels, contrast agent enemas are rarely performed in practice, but have special indications. A cause of the intestinal atony should be found quickly in order to assess the severity and the need for action.
When should you go to the doctor?
If symptoms such as nausea and vomiting, or constipation occur, the patient may have a serious gastrointestinal tract disease. A doctor should therefore be consulted immediately in the event of the complaints mentioned. The doctor can determine intestinal atony on the basis of a physical examination and take the necessary steps. Treatment is necessary in any case and can prevent complications if it is done early. However, if the intestinal paralysis remains untreated, a medical emergency can arise.
For example, it can lead to an intestinal infarction, which in the worst case leads to the death of the patient. Constipation and a bloated stomach are signs of such a severe course. If you notice these symptoms, it is best to contact the emergency doctor immediately.
Depending on how far the intestinal atony has progressed, a longer hospital stay may be necessary. In order to avoid further complications and a recurrence of intestinal paralysis, the causes of the symptoms must be determined. The right contact person for this is the gastroenterologist or a nutritionist.
Doctors & therapists in your area
Treatment & Therapy
There are some emergencies associated with intestinal atony that require immediate therapy:
In mesenteric infarction caused by blood flow, for example, intestinal tissue dies every minute; the intestine can only be saved with interventional measures or open surgery if intervention is timely. If too much intestinal tissue has already died, it can no longer be replaced; in the worst case, the person affected is no longer viable.
In all the other cases of disease-accompanying or post-operative intestinal atony, gentle measures can be used to stimulate the intestinal activity. In addition to a careful diet, this includes enemas in particular, but also drug attempts (e.g. with the parasympathomimetic neostigmine).
Outlook & forecast
The prognosis is determined according to the cause and thus the underlying disease of the intestinal paralysis. The sooner the patient receives medical treatment, the better the chances of recovery. Without proper care, there is a significant deterioration in health and, under certain circumstances, a life-threatening condition can occur.
If the treatment is successful, bowel function returns to normal after a few days or weeks. There is then no symptoms and the patient is discharged from the treatment as cured. In some cases, there is a chance that normal bowel function will be restored within a few hours of receiving medical attention.
With a healthy diet adapted to the needs of the weakened body, the patient can make a significant contribution to building up his health. Pollutants such as nicotine or alcohol as well as the intake of fatty foods should be avoided. The healing process is facilitated and the intestinal activity is gently stimulated with an adapted diet. Intestinal atony can recur in the course of life.
The prognosis is unchanged when it comes back. The disease can be optimally countered with a healthy lifestyle and a balanced diet. In many cases, successful prevention and permanent recovery are possible.
prevention
Prevention of intestinal atony is specifically not possible and would have to start with the prevention of the underlying diseases (e.g. a healthy lifestyle to avoid arteriosclerosis, no alcohol abuse to avoid pancreatitis, etc.).
Aftercare
In most cases of intestinal atony, the patient has only a few measures and options for follow-up care. In the case of this disease, the person affected must first and foremost consult a doctor so that there are no further complications or, in the worst case, even death of the person concerned. The earlier the intestinal atony is recognized and treated, the better the further course of this disease is usually.
The patient should therefore consult a doctor at the first signs and symptoms of intestinal atony. An emergency doctor can also be called in an emergency. The treatment itself takes the form of a surgical procedure. After this procedure, the person affected should rest and take care of their body. Strict bed rest is to be observed.
Most of those affected depend on the help and care of their own family and friends. This care usually has a positive effect on the course of the disease and can also prevent psychological upsets or depression. After the procedure, fatty or very sweet foods should be avoided. Whether this disease will lead to a reduced life expectancy for the patient cannot generally be predicted.
You can do that yourself
Measures that sufferers of intestinal atonia can take themselves are limited to positive stimulation of the intestinal activity that is still present and to contain risk factors. A well-advanced intestinal paralysis that is already leading or leading to an occlusion or has caused tissue damage cannot be improved without medical means.
Those affected are encouraged to adjust their diet to two things: On the one hand, it must be easy to digest and encourage smooth and regular stool. This includes eating enough fiber, fluids, and a healthy diet in general.
Second, the diet must prevent or counteract arteriosclerosis. This is achieved with little alcohol, little processed fats, and enough antioxidants and vitamins. This regulates digestion and reduces the tendency to develop arteriosclerosis.
Food should also be consumed in well-chewed, small portions. Meals should be spread over the day. In addition, the normal amount of food should only be consumed again when the intestine is at all working again.
Enemas - possibly with mild substances - can stimulate intestinal activity. Warmth, moderate and regular exercise, and relaxing baths can also help. When taking the measures, it is relevant to consider the cause of the intestinal paralysis.

.jpg)
.jpg)
.jpg)






.jpg)



.jpg)










.jpg)
