As Duodenitis Doctors call inflammation of the duodenal lining. It can take an acute as well as a chronic course.
What is duodenitis?

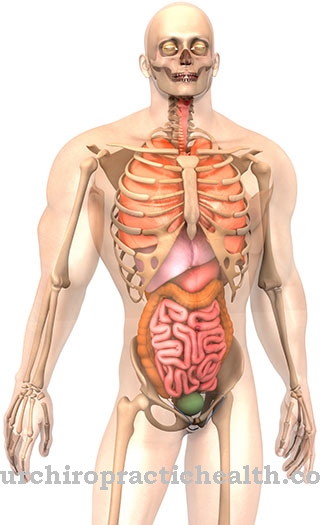
© peterjunaidy - stock.adobe.com
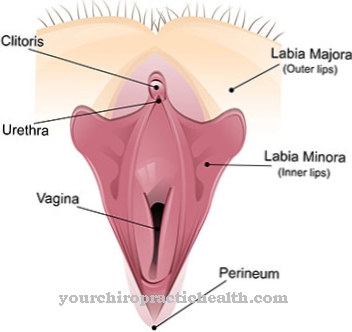
Duodenitis is inflammation of the lining of the duodenum (duodenum). The name duodenum goes back to the fact that this part of the body is about twelve fingers wide.
The duodenum is part of the intestinal tube and is directly connected to the gastric porter. As a curve in the shape of a C, the duodenum represents the beginning of the small intestine. The task of the duodenum is to neutralize the gastric hydrochloric acid that is transported from the stomach to the intestine along with food.
causes
Duodenitis can be caused by different triggers. These include primarily infections of the intestinal tract that are caused by viruses, bacteria such as Shigella or Salmonella, and amoebas. One of the most common causes of duodenitis is the bacterium Helicobacter pylori, which often lodges in the stomach in childhood and causes symptoms in around ten percent of all those affected.
The bacterium has the ability to produce ammonia. This can irritate the surface lining in the small intestine and ultimately cause inflammatory reactions. If the surface layer of the mucous membrane is penetrated, there is a risk of a duodenal ulcer. However, harmful substances such as certain medications, including nonsteroidal anti-inflammatory drugs such as acetylsalicylic acid (ASA), diclofenac, naproxen and ibuprofen, can have a damaging effect on the lining of the duodenum.
This is especially true for long-term use. In rare cases, inflammatory bowel disease, Crohn's disease, is the cause of duodenitis. Other possible causes include diseases of the stomach, biliary tract or pancreas, disorders of the central nervous system, stress and exposure to alcoholic beverages.
You can find your medication here
➔ Medicines for stomach ailments and painSymptoms, ailments & signs
Duodenitis is noticeable in different ways. In many cases, it is not even noticed by those affected, so that a diagnosis is only made by chance. Typical symptoms of duodenitis are stabbing or pressing pain that occurs under the costal arch, loss of appetite, digestive problems, as well as nausea and vomiting.
If there is a duodenal ulcer, the symptoms are particularly evident between meals. However, they can also appear when fasting and get better after a meal, which reduces the pain after meals.
In the case of chronic duodenitis or a duodenal ulcer, black or bloody stools and intense abdominal pain are not uncommon. As this can indicate an intestinal bleeding, a doctor should be consulted quickly in such cases.
Diagnosis & course
If the symptoms of duodenitis are brought to a doctor, he or she will usually first perform a sonography (ultrasound examination) or have X-rays taken. He also has the option of performing a duodenoscopy, which, like gastroscopy, involves mirroring with an endoscope.
The endoscope is equipped with a thin tube and a camera. The doctor inserts this instrument through the esophagus and stomach into the duodenum. With the help of the camera, recordings are made that can be played back on a connected monitor. Using a small instrument attached to the tube of the endoscope, the doctor can take samples from the wall of the duodenum, which is called a biopsy.
A clear sign of duodenitis is swelling on the uppermost intestinal wall mucosa. In addition, gastric mucosal cells are found within the duodenum. The doctor can recognize severe forms of duodenitis by atrophy (thinning). An ulcer can be identified as a well-defined inflammation.
A duodenoscopy can be followed by the patient while they are awake. But it is also possible to give him a surface anesthetic. Duodenitis usually takes a positive course and after a few days, with appropriate medical treatment, symptoms are free again. However, if the cause of the ailment cannot be determined, the inflammation can always return.
Complications
With duodenitis, complications need not always arise. Often the person concerned does not even notice the inflammation if it is not discovered by chance during an examination. In other cases, the inflammation causes pain in the abdomen and loss of appetite.
Vomiting and nausea also occur and can thereby reduce the patient's quality of life. Symptoms particularly affect the patient between meals. In some cases, intestinal bleeding also causes bloody stools. This can lead to a panic attack in many people.
Duodenitis can be treated and limited well. If the inflammation occurs from taking painkillers, they must be stopped or replaced with another drug. Usually there is a quick improvement without complications.
The inflammation itself is fought with the help of antibiotics and usually proceeds without any further symptoms. However, the patient has to adjust to a change in diet and is limited to a few foods during treatment. Life expectancy is not reduced by duodenitis.
When should you go to the doctor?
In any case, a doctor must be consulted with duodenitis. This disease does not self-heal, so early treatment can avoid possible complications and other complaints. A doctor should be consulted if there is severe and, above all, chronic pain in the intestinal area that cannot be attributed to gastrointestinal flu. Indigestion or loss of appetite can also indicate duodenitis and should be examined if it occurs for a long time.
It is also advisable to consult a doctor if vomiting and nausea persist. This can lead to significant discomfort, especially between meals. An immediate visit to the doctor is necessary if the duodenitis has resulted in bloody stools. In emergencies or in very severe pain, a hospital should be visited or the emergency doctor should be called directly. Usually, duodenitis is treated by and can be diagnosed by an internist.
Doctors & therapists in your area
Treatment & Therapy
When treating duodenitis, the focus is on combating the underlying cause. If the inflammation of the duodenum was triggered by the use of pain relievers, it is advisable to replace them with other drugs. If, on the other hand, the bacterium Heliobacter pylori causes the disease, its colonization of the gastrointestinal tract must be stopped, which means that the inflammation is treated indirectly.
Such treatment can take seven to ten days to complete. A so-called proton pump inhibitor (stomach acid blocker) is administered to the patient. He is also given a combination of two antibiotics such as metronidazole, clarithromycin or amoxicillin. In most cases, the duodenum will recover from the inflammation after this treatment.
In some patients, a reduction in gastric acid production is sufficient. The sensitive mucous membrane of the duodenum is often affected by the hydrochloric acid, which is produced in the stomach. The stomach acid can be reduced through a gentle diet with low-fat, mild whole food that is easy to digest.
In contrast, high-fat foods have a stimulating effect on gastric acid production and put a strain on the gastrointestinal tract. To support the duodenum, natural remedies such as mustard seeds, aloe with sugar water or plantain juice mixed with honey can also be taken.
Outlook & forecast
In most cases, duodenitis can be treated relatively well, so that there are no particular complications for the person concerned. Early diagnosis and treatment always have a positive effect on the further course of the disease.
If the duodenitis is not treated, the affected person will suffer from severe abdominal pain and bloody stools. The symptoms usually increase and there is no self-healing. As the disease progresses, bleeding occurs in the intestine and an ulcer forms. The inflammation can also spread to the surrounding organs, so that immediate treatment is necessary.
Treatment is in most cases with the help of medication and can completely alleviate the symptoms. The duodenum usually recovers after successful treatment, so there is no long-term damage. A balanced and healthy diet can also have a positive effect on the course of the disease. Surgery is only necessary in severe cases to treat duodenitis. Therefore, life expectancy is usually not reduced with this disease.
You can find your medication here
➔ Medicines for stomach ailments and painprevention
In order to prevent duodenitis, a healthy lifestyle is recommended, which consists of easily digestible whole foods. It also makes sense to refrain from alcohol, tobacco and drugs that can damage the gastrointestinal tract.
Aftercare
In most cases, the measures and options for follow-up care for duodenitis are very limited. A comprehensive examination and diagnosis of the disease must first take place so that there are no further complications or further complaints for the person concerned. The earlier the duodenitis is recognized and treated, the better the further course of the disease will usually be.
In most cases of duodenitis, those affected are dependent on taking medication to alleviate the symptoms. It is important to ensure the correct dosage and regular intake. As a rule, the instructions of the doctor should be followed, although a doctor should be contacted if you have any questions or if in doubt.
Not infrequently, a healthy lifestyle with a balanced diet can also have a positive effect on the course of duodenitis and significantly alleviate the symptoms. The person affected should avoid fatty or very sweet foods in order to protect the intestines and stomach. Whether duodenitis will reduce the patient's life expectancy cannot generally be predicted.
You can do that yourself
The course of the disease and the severity of duodenitis depend on the causative factors and the possibility of getting rid of them. Self-help measures and an adaptation of the behavior in everyday life can support a positive course of the disease in terms of severity and duration.
In cases where the duodenitis was caused by long-term use of pain relievers and nonsteroidal anti-inflammatory drugs such as diclofenac, ibuprofen, or acetylsalicylic acid (aspirin), stopping the drugs can lead to rapid improvement and regeneration of the lining of the duodenum (duodenum).
In some cases, a change in diet to a low-fat, light diet is sufficient to reduce gastric acid production, which is strongly stimulated in high-fat diets and leads to inflammation in the intestinal lining of the duodenum. The change in diet can also take place as an accompanying measure parallel to treatment with so-called proton pump inhibitors.
If the symptoms were caused by a bacterial or viral infection, which indicate a weakening of the immune system, the diet should be aimed at strengthening the immune system in addition to drug therapy. Before the supply of vitamins, minerals and various enzymes has a positive effect, so that the pathogenic germs can also be better combated by the immune system. Refraining from any alcohol or tobacco consumption during the treatment of duodenitis also has a positive effect.








.jpg)

.jpg)
.jpg)











.jpg)