A healthy one Intestinal lining plays an important role in the human body. If it is damaged, this can manifest itself in various symptoms and clinical pictures.
What is the intestinal lining?
The Intestinal lining, which are also called Mucosa called, lines the intestine and is the innermost of four layers of the intestinal wall. The intestinal mucosa is built up slightly differently in the individual intestinal sections, which means that it is adapted to the different functions of the small intestine, large intestine and rectum. It has important functions in digestion, protection against pathogens and for the immune system.
Anatomy & structure
The intestinal mucosa rests on a layer of connective tissue that is surrounded by smooth muscles. Nerve fibers are located between the intestinal mucosa and these muscles. The intestinal mucosa is made up of three layers. It consists of a single columnar epithelium, the Lamina epithelialis mucosae. The columnar epithelium is a specific form of the epithelium that takes its name from the elongated, cylindrical cells. The second layer is the so-called Lamina propria mucosae, a connective tissue layer with lymph and blood vessels as well as nerve fibers and immune cells. The third layer is a muscle layer called the lamina muscularis mucosae. This muscle layer is responsible for the intrinsic mobility of the intestinal mucosa.
The epithelial cells of the lamina epithelialis mucosae carry so-called microvilli, which are also known as brush borders and serve to enlarge the surface. Due to the folds of the intestinal mucous membrane with the brush border of the lamina epithelialis mucosae, the surface reaches a size of approximately 200 square meters.
The brush border is surrounded by a so-called glycocalyx to prevent self-digestion. The glycocalyx is made up of polysaccharides and is located on the outside of all cells. However, it differs in composition and structure between different cells, which determines their specific function. In addition to its main task of protecting against self-digestion, the glycocalyx of the intestinal mucosa is involved in the absorption of nutrients and contains digestive enzymes.
Function & tasks
The main task of the intestinal mucosa is to absorb components from food and water. For this purpose, cells of the intestinal mucosa form specific enzymes that split nutrients so that they can be absorbed and released into the blood. Here, the food components are absorbed either through active or passive absorption.
In passive resorption, the food components come from the interior of the intestine, where they are present in high concentration, through osmosis in cells of the intestinal mucosa with a low concentration. With active absorption, the food components can also reach cells of the intestinal mucosa with the same or higher concentration of nutrients while consuming energy.
The intestinal mucosa also protects against the ingress of harmful bacteria and parasites from food and the environment. It is colonized by numerous microorganisms that are useful for the body, known as the intestinal flora. There are around 400 to 500 different bacterial strains in the healthy intestinal flora, but these only settle after birth and are not yet present in the newborn baby.
The intestinal flora prevents harmful microorganisms from settling on the mucous membrane, modulates and stimulates the immune system, supplies the mucous membrane with nutrients and promotes the metabolism. In addition, some bacterial strains in the intestinal flora produce important vitamins.
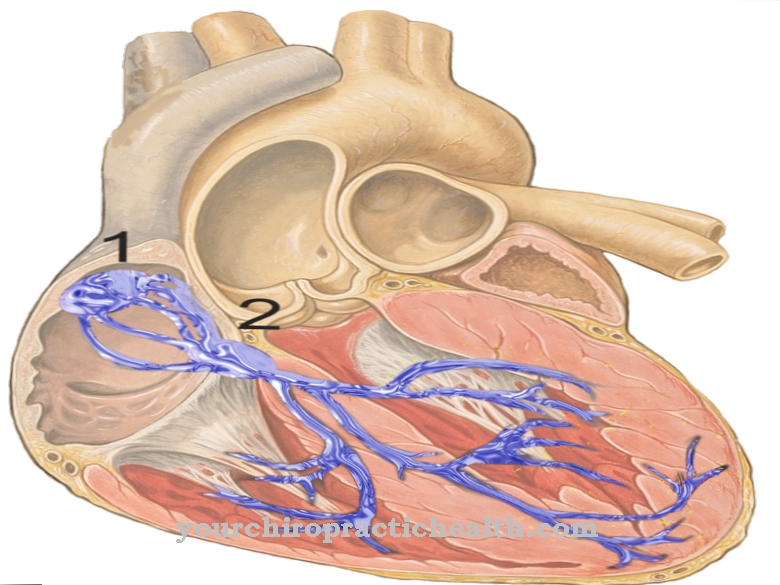
The intestinal lining is an important part of the immune system as it contains more than 70 percent of the body's antibody-producing cells. It is therefore referred to as the gut-associated immune system. When pathogens penetrate, the antibodies bind to them so that the pathogens are recognized and destroyed by specific cells of the immune system.
The immune system can differentiate between the bacteria of the healthy intestinal flora, food components and harmful substances or pathogens. Specific cells of the intestinal mucosa also produce various hormones that control the functions of the gastrointestinal area.
Illnesses & ailments
An unhealthy diet, the use of medication such as antibiotics, cortisone or radiation or chemotherapy can unbalance the intestinal flora, as can the use of painkillers over a longer period of time, psychological stress and stress.
If the intestinal flora is damaged over a longer period of time, this leads to changes in the intestinal mucous membrane and this becomes permeable to toxic substances or incompletely digested food components.
Intestinal functions are disturbed and harmful germs can spread. If pathogens displace the beneficial microorganisms of the intestinal flora, we speak of a dysbiosis or dysbacteria. Symptoms can include belching, flatulence, intestinal cramps or colic. Disorders or damage to the intestinal mucosa can be the cause of many different clinical pictures due to the diverse functions.
In addition to chronic inflammatory bowel diseases such as intestinal mucosal inflammation, Crohn's disease or ulcerative colitis, allergies or a weakened immune system can be the result. In Crohn's disease, the inflammation can affect the entire digestive tract; in ulcerative colitis, the inflammation is limited to the colon and rectum. If only the appendix is affected by inflammation, it is appendicitis.
Since untreated inflammation of the mucous membrane can lead to serious diseases such as colon cancer, symptoms must be taken seriously and, if necessary, consult a doctor. The ingestion of pathogens through bad food or contaminated drinking water can lead to intestinal infections from pathogens that damage the intestinal mucosa.
Classic symptoms are diarrhea, abdominal pain, and loss of appetite. Typhoid and cholera pathogens, for example, are triggers of particularly severe intestinal infections. Another disease of the intestinal mucosa is celiac disease. The mucous membrane of the small intestine is intolerant to gluten, a cereal protein.



.jpg)


.jpg)


.jpg)




.jpg)