Mycobacteria are a genus within the family Mycobacteriaceae and the order Actinomycetales. They include pathogens such as Mycobacterium tuberculosis, which can cause tuberculosis in humans.
What are mycobacteria?
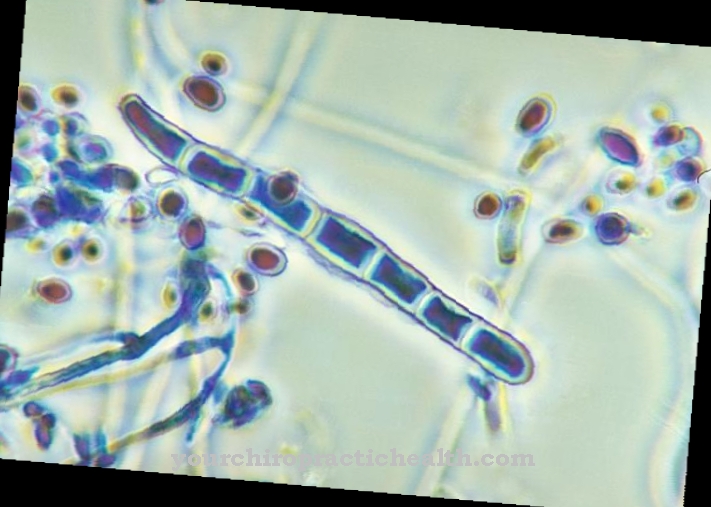
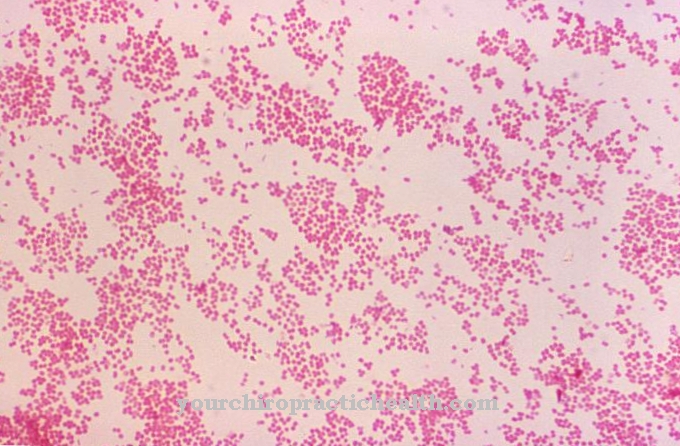
Mycobacteria are gram-positive aerobic bacteria. They are acid-resistant, rod-like and cannot move on their own. Aerobic means that the bacteria depend on oxygen. They also need organic substances to generate energy.
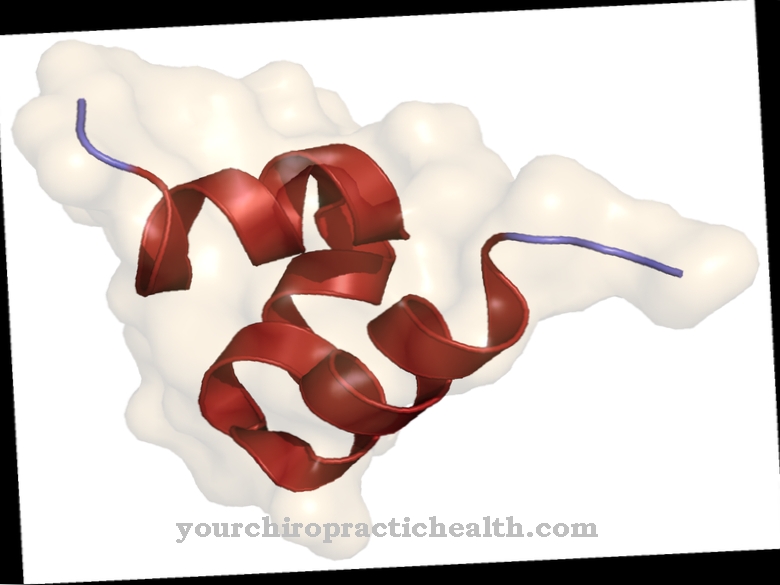
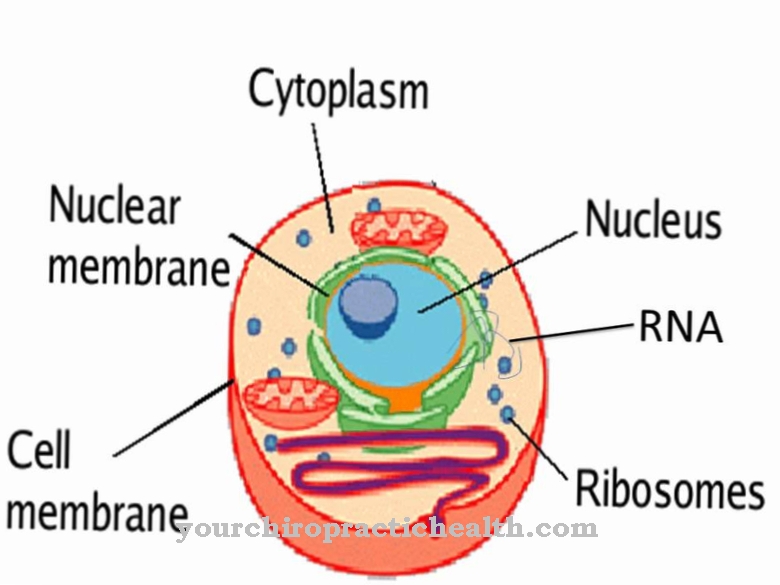
A distinctive feature of the mycobacteria is their cell wall. Much of the cell wall acts as an antigen component. As a result, mycobacteria in the infected organisms cause a reaction of the immune system. This leads to a type IV allergy. It is a late-type allergy. The best-known late allergic reaction to a mycobacterium is the tuberculin reaction, which is also used in the context of tuberculosis diagnostics in the form of the tuberculin test. The high lipid content of the cell wall is also typical. Together with the mycolic acids, it ensures that the bacterium has a high acid resistance.
Due to the specific structure of the cell wall, mycobacteria are very resistant. They can also remain infectious for several months outside of their host under favorable conditions. With a few exceptions, they are resistant to most antibiotics. Most alkalis and acids cannot harm mycobacteria either. The acid resistance can be proven with the help of the Ziehl-Neelsen staining. Only bacterial species such as Nocardia or Corynebacterium have a similar acid resistance.
Occurrence, Distribution & Properties
Around 100 species belong to the group of mycobacteria. Most of these bacteria are non-pathogenic. This means that they do not cause disease in humans. They occur freely in the environment and are classified as non-tubercular mycobacteria. These bacteria feed by decomposing dead organic matter. They can be detected in dust, sea water, fresh water, in the soil and in groundwater. An example of such mycobacteria are the mycobacteria of the Mycobacterium terrae complex and the Mycobacterium fortuitum. The species Mycobacterium gordnoae or Mycobacterium chelonae can be found in drinking water. Most pathogenic mycobacteria belong to the obligate pathogenic Mycobacterium tuberculosis complex. They live within phagocytes (macrophages) and are therefore parasites.
The mycobacteria that can cause tuberculosis are found around the world. According to the World Health Organization (WHO), a third of the world's population is infected with the bacteria. A new case of tuberculosis occurs every second. However, only a small proportion of the infections actually lead to an outbreak of the disease. There are around 4,000 cases of tuberculosis in Germany every year. However, the number of unreported cases is quite high. The disease is particularly widespread in Germany in Bremen, Berlin and Hamburg.
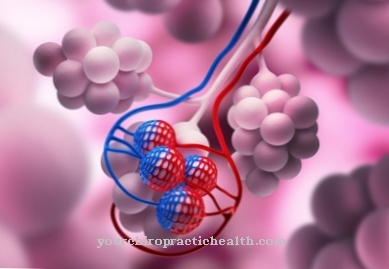
Tuberculosis is most commonly transmitted through inhalation of infectious aerosols. This transmission path is also known as droplet infection. For an infection with the mycobacteria, it is sufficient to inhale a few very small microdroplets, each of which contains only one to three pathogens. Transmission via the bloodstream is also possible. However, this transmission route is rather rare. Infection from contaminated food used to be quite common. Since milk has been pasteurized, intestinal tuberculosis is hardly ever found in humans in Germany.
The infection with the tuberculosis pathogens can also occur sexually or through smear infections. Furthermore, if the uterus is infected, the bacteria can also be transmitted to the child. The same applies to urogenital tuberculosis. Transmission during the birth process is also possible here.
You can find your medication here
➔ Medicines against coughs and coldsIllnesses & ailments
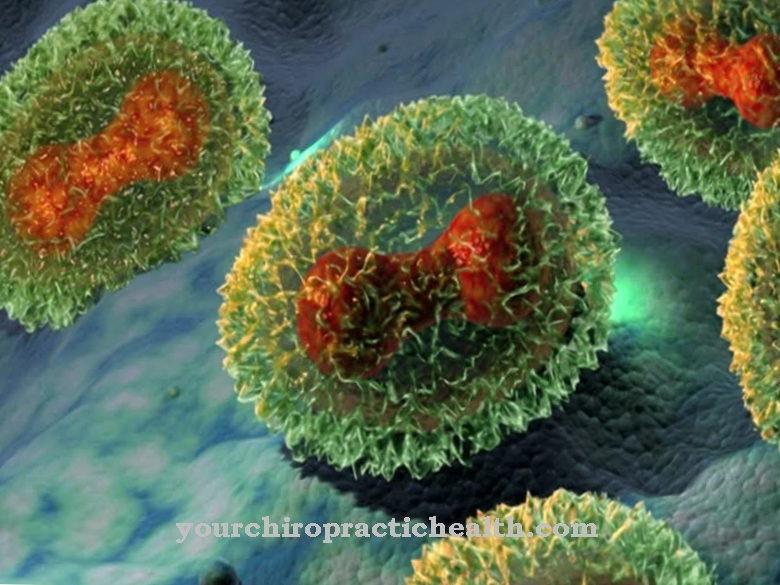
The most important causative agent of tuberculosis is Mycobacterium tuberculosis. Most infections are fended off by the immune system in the airways. Only a tenth of all infected people develop tuberculosis. Whether the disease breaks out depends primarily on the state of the immune system. The nutritional status, the amount of bacteria ingested and the frequency of contact with the pathogens also play a role. In the alveoli, the mycobacteria meet the phagocytes of the lungs (alveolar macrophages). The pathogens can absorb these, but due to the special cell wall they cannot destroy them. This is why the body's immune system forms a kind of protective wall around the source of infection. This protective wall consists of macrophages, giant Langhans cells, epithelial cells and lymphocytes. A focus of inflammation with a central necrosis (tissue destruction) develops within this wall. The structure of immune cells and inflammation focus is also known as tubercular granuloma. The mycobacterium is isolated within this protective wall and cannot cause any further damage. It is hindered from spreading by the immune cells, but can live within the wall for decades. If the immune system is not as strong as it was at the beginning of the infection, the protective wall can break open and the bacteria are set free. Reinfection occurs and, if the immune system is in a very poor condition, miliary tuberculosis occurs.
In principle, the course of tuberculosis can be divided into stages. The first signs of the disease are called primary tuberculosis. This stage is associated with uncharacteristic symptoms such as loss of appetite, night sweats, fever and fatigue. Other symptoms are coughing without sputum and hoarseness. If the bacteria spread in the blood, a severe clinical picture with fever, weight loss, cough and shortness of breath develops. Tuberculous meningitis, an inflammation of the meninges, can also develop. If the immune system is extremely weak, sepsis can develop, which is usually fatal.
In ten percent of all infected people, the disease only breaks out later as secondary tuberculosis. Typical symptoms of secondary tuberculosis are persistent cough with mucous sputum, fatigue, night sweats, chest pain and shortness of breath.








.jpg)


.jpg)

.jpg)